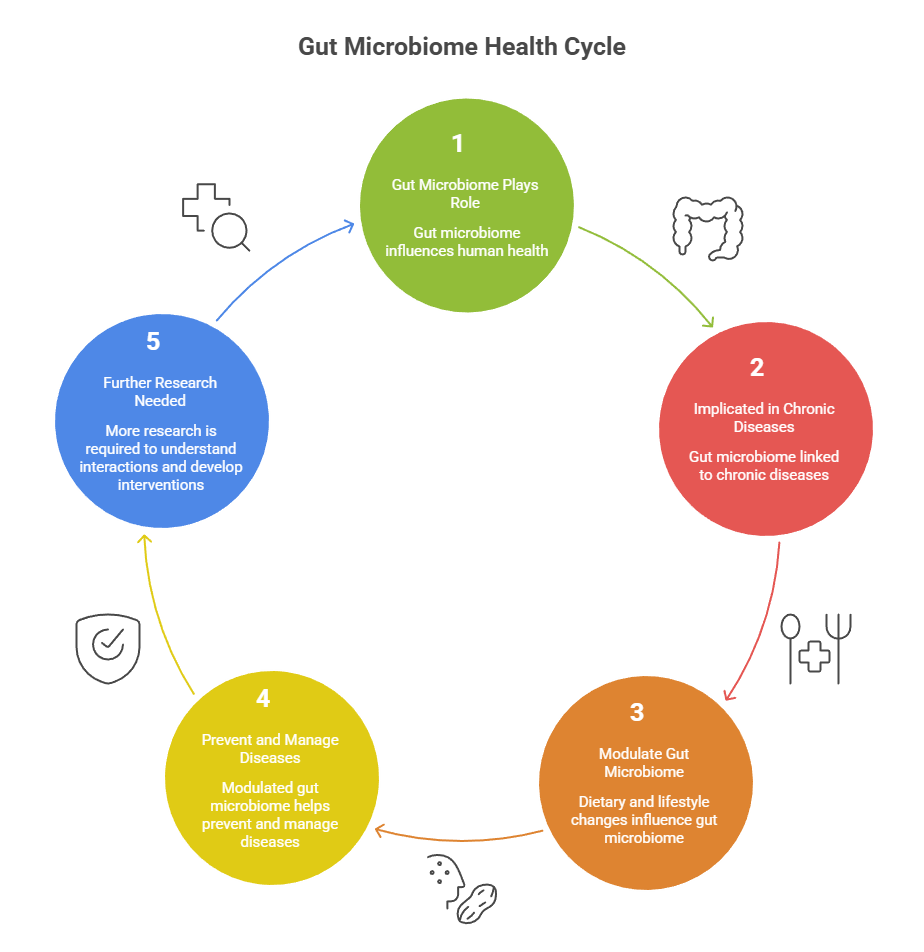
The gut microbiome — the trillions of bacteria, fungi, and other microorganisms in our digestive tract — has emerged as a central regulator of human health. Far from being a digestive sidebar, its balance and diversity influence inflammation, metabolism, immune function, and chronic disease progression. Recent research confirms its role in preventing and managing chronic noncommunicable diseases such as diabetes, cardiometabolic disease, inflammatory bowel disease (IBD), and even cancer therapy responses.
Why the Gut Microbiome Matters in Chronic Disease
Scientific evidence indicates that microbial diversity and composition directly impact:
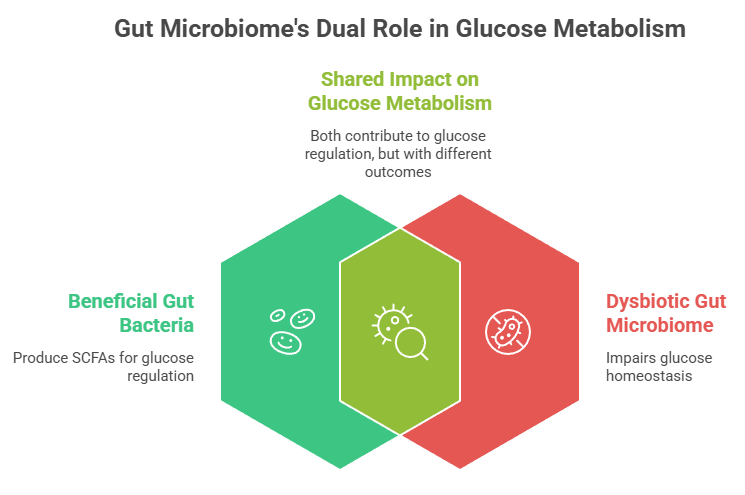
- Metabolic regulation: Beneficial bacteria produce short‑chain fatty acids (SCFAs) that improve glucose metabolism and reduce systemic inflammation.
- Immune modulation: A balanced microbiome helps regulate immune responses and reduce chronic inflammatory states linked to conditions such as rheumatoid arthritis and metabolic syndrome.
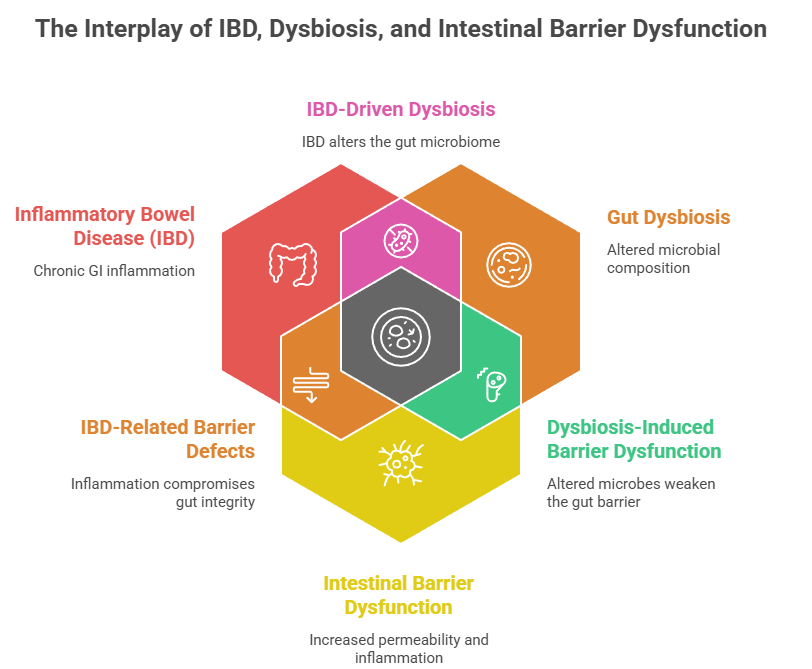
- Barrier integrity: Healthy microbiomes strengthen the gut barrier, lowering “leaky gut” risk—a trigger for systemic inflammation and chronic disease.
Gut Microbiome & Metabolic Pathways — Key Insights
Studies have correlated gut dysbiosis (imbalanced microbiota) with higher risks for obesity, type 2 diabetes, hypertension, and non‑alcoholic fatty liver disease.
Evidence‑Backed Programs for Gut Microbiome Health
1. Dietary Patterns That Promote Microbiome Diversity
Broad dietary interventions consistently outperform single‑strain supplements in improving metabolic and inflammatory markers:
- High‑fibre, plant‑rich diets increase SCFA‑producing bacteria and lower inflammatory signaling.
- Mediterranean and other whole‑food diets correlate with higher levels of beneficial genera and reduced cardiometabolic risk.
These changes are linked not just to microbial shifts but measurable improvements in blood glucose, lipid profiles, and inflammatory biomarkers.
Practical takeaways:
• Eat whole grains, legumes, fruits, and vegetables daily.
• Prioritize fibre to nourish SCFA producers like Faecalibacterium and Roseburia.
2. Prebiotics & Synbiotics: Targeted Functional Foods
Unlike isolated probiotics, prebiotics (non‑digestible fibres that feed beneficial microbes) and synbiotics (combined probiotics + prebiotics) show stronger clinical effects:
- Reduced insulin resistance and inflammation in metabolic syndrome.
- Enhanced abundance of health‑associated bacteria and better glycemic control.
These improvements translate into measurable clinical outcomes like decreased HbA1c in prediabetes and lower circulating endotoxin levels—a driver of chronic inflammation.
3. Fecal Microbiota Transplantation (FMT): A Therapeutic Frontier
FMT — transferring gut microbes from healthy donors to patients — is the most effective microbiome‑based therapy to date for certain conditions:
- It reduces recurrence rates of Clostridioides difficile infection (CDI) by up to 93 %, a major clinical success.
- Early trials show FMT can influence outcomes in ulcerative colitis and possibly enhance cancer immunotherapy responses by modulating immune signaling.
Although research is ongoing, FMT represents a shift from symptom management to microbiome‑directed treatment with clear clinical endpoints.
4. Precision Nutrition & Personalized Microbiome Strategies
Individual responses to the same diet or supplement can vary widely due to unique microbiome compositions. Precision nutrition programs — using microbiome profiling to tailor diet and lifestyle guidance — are gaining traction and show promise for:
- Reducing cardiometabolic risk.
- Enhancing immune modulation based on specific bacterial signatures.
This personalized approach moves beyond one‑size‑fits‑all advice to targeted, data‑driven preventive care.
What This Means for Chronic Disease Prevention
Interstitial research emphasizes that successful programs combine diet, lifestyle, and targeted interventions to support a resilient gut ecosystem rather than relying on quick fixes like juice cleanses or single‑strain probiotics alone.
Key Action Points
✔ Increase dietary fibre and polyphenol‑rich foods.
✔ Use prebiotic and synbiotic formulations with proven clinical benefits.
✔ Consider advanced interventions like FMT under medical supervision for specific indications.
✔ Explore personalized microbiome profiling for tailored preventive strategies.
Conclusion
The gut microbiome is no longer an abstract concept; it’s a clinically relevant target for chronic disease prevention and management. Evidence‑backed programs that integrate dietary patterns, functional foods, microbiome therapy, and personalized nutrition deliver measurable health benefits—improving metabolic profiles, lowering inflammation, and enhancing chronic disease outcomes.
By prioritizing long‑term microbiome health, health systems and individuals can shift from reactive disease treatment to proactive prevention.
FAQs:
1. How does gut microbiome composition influence host glucose and insulin signaling pathways?
The gut microbiome influences glucose homeostasis through microbial metabolites (notably SCFAs), modulation of incretin hormones (GLP-1, GIP), and regulation of systemic inflammation. Beneficial taxa such as Akkermansia muciniphila and Faecalibacterium prausnitzii improve insulin sensitivity by enhancing gut barrier integrity and reducing endotoxemia, while dysbiosis increases lipopolysaccharide (LPS)-mediated insulin resistance.
2. What role do short-chain fatty acids (SCFAs) play in regulating lipid and energy metabolism?
SCFAs—acetate, propionate, and butyrate—are produced by microbial fermentation of dietary fiber. They activate G-protein–coupled receptors (GPR41, GPR43), regulate hepatic lipogenesis, improve insulin sensitivity, and enhance mitochondrial energy utilization. Butyrate also supports intestinal epithelial health and reduces metabolic inflammation.
3. How does dysbiosis contribute to insulin resistance and type 2 diabetes mellitus?
Dysbiosis increases gut permeability, allowing translocation of microbial endotoxins (metabolic endotoxemia). This triggers chronic low-grade inflammation via TLR4 signaling, impairing insulin receptor signaling in liver, muscle, and adipose tissue. Reduced SCFA-producing bacteria further worsen insulin resistance.
4. Which microbial metabolites directly modulate hepatic metabolic pathways?
Key metabolites include SCFAs, secondary bile acids, indole derivatives, and trimethylamine (TMA). These compounds influence hepatic gluconeogenesis, lipid oxidation, cholesterol metabolism, and inflammatory signaling via FXR, PPAR-α, and AhR pathways.
5. Can alterations in the gut microbiome affect mitochondrial function and cellular energy balance?
Yes. Microbial metabolites such as butyrate enhance mitochondrial biogenesis and oxidative phosphorylation. Dysbiosis impairs mitochondrial efficiency, increases oxidative stress, and shifts energy metabolism toward glycolysis, contributing to metabolic disease progression.
6. How does the gut microbiome regulate bile acid metabolism and FXR/TGR5 signaling?
Gut bacteria convert primary bile acids into secondary bile acids, which act as signaling molecules for FXR and TGR5 receptors. These pathways regulate glucose metabolism, lipid homeostasis, insulin sensitivity, and energy expenditure. Dysregulated bile acid signaling is implicated in NAFLD and metabolic syndrome.
7. What is the impact of antibiotics on gut microbiome–mediated metabolic regulation?
Antibiotics disrupt microbial diversity, reduce SCFA production, and alter bile acid metabolism. Early-life or repeated antibiotic exposure is associated with increased risk of obesity, insulin resistance, and metabolic dysregulation due to long-term microbiome imbalance.
8. How does gut microbiota–driven inflammation disrupt host metabolic homeostasis?
Pro-inflammatory microbial profiles increase cytokines such as TNF-α and IL-6, which interfere with insulin signaling pathways. Chronic inflammation alters adipocyte function, promotes hepatic steatosis, and worsens systemic metabolic control.
9. Are specific microbial taxa associated with obesity, metabolic syndrome, or NAFLD?
Yes. Reduced abundance of Akkermansia muciniphila and Bacteroidetes, along with increased Firmicutes and endotoxin-producing Proteobacteria, is commonly observed in obesity and NAFLD. These shifts influence energy harvest, fat storage, and inflammation.
10. How does the gut microbiome interact with endocrine hormones such as GLP-1, PYY, and leptin?
Microbial metabolites stimulate enteroendocrine cells to release GLP-1 and PYY, improving insulin secretion and appetite regulation. Dysbiosis impairs this signaling and contributes to leptin resistance, promoting weight gain and metabolic dysfunction.
11. Can gut microbiome modulation improve metabolic outcomes in prediabetes and obesity?
Clinical studies suggest that dietary fiber, prebiotics, probiotics, and lifestyle interventions can favorably modify the gut microbiome, improving insulin sensitivity, reducing inflammation, and supporting weight management, particularly in early metabolic disease.
12. What is the clinical significance of gut microbiome–derived trimethylamine N-oxide (TMAO) in cardiometabolic disease?
Elevated TMAO levels are associated with increased cardiovascular risk, atherosclerosis, and insulin resistance. TMAO alters cholesterol metabolism and promotes vascular inflammation, making it a potential biomarker and therapeutic target in cardiometabolic disease.
13. How do dietary interventions reshape gut microbiome–host metabolic interactions?
Diet is a primary modulator of the microbiome. High-fiber, plant-rich diets increase SCFA-producing bacteria, while high-fat, ultra-processed diets promote dysbiosis. Dietary changes can rapidly improve microbial diversity and metabolic signaling pathways.
14. Are fecal microbiota transplantation (FMT) or targeted probiotics effective for metabolic disorders?
FMT has shown short-term improvements in insulin sensitivity in select trials, but long-term efficacy remains uncertain. Targeted probiotics and synbiotics show modest metabolic benefits and are currently adjunctive rather than primary therapies.
15. How can gut microbiome profiling be integrated into personalized metabolic medicine?
Microbiome profiling may help stratify metabolic risk, guide dietary interventions, and predict therapeutic response. While promising, its clinical use remains adjunctive due to variability, cost, and lack of standardized reference ranges.
Dr. Mohammed Abdul Azeem Siddiqui, MBBS, M.Tech (Biomedical Engineering – VIT, Vellore)
Registered Medical Practitioner – Reg. No. 39739
Physician • Clinical Engineer • Preventive Diagnostics Specialist
Dr. Mohammed Abdul Azeem Siddiqui is a physician–engineer with over 30 years of dedicated clinical and biomedical engineering experience, committed to transforming modern healthcare from late-stage disease treatment to early detection, preventive intelligence, and affordable medical care.
He holds an MBBS degree in Medicine and an M.Tech in Biomedical Engineering from VIT University, Vellore, equipping him with rare dual expertise in clinical medicine, laboratory diagnostics, and medical device engineering. This allows him to translate complex laboratory data into precise, actionable preventive strategies.
Clinical Mission
Dr. Siddiqui’s professional mission centers on three core pillars:
Early Disease Detection
Identifying hidden biomarker abnormalities that signal chronic disease years before symptoms appear — reducing complications, hospitalizations, and long-term disability.
Preventive Healthcare
Guiding individuals and families toward longer, healthier lives through structured screenings, lifestyle intervention frameworks, and predictive diagnostic interpretation.
Affordable Evidence-Based Treatment
Delivering cost-effective, scientifically validated care accessible to people from all socioeconomic backgrounds.
Clinical & Technical Expertise
Across three decades of continuous practice, Dr. Siddiqui has worked extensively with:
Advanced laboratory analyzers and automation platforms
• Cardiac, metabolic, renal, hepatic, endocrine, and inflammatory biomarker systems
• Preventive screening and early organ damage detection frameworks
• Clinical escalation pathways and diagnostic decision-support models
• Medical device validation, calibration, compliance, and patient safety standards
He is recognized for identifying subclinical biomarker shifts that predict cardiovascular disease, diabetes, fatty liver, kidney disease, autoimmune inflammation, neurodegeneration, and accelerated biological aging long before conventional diagnosis.
Role at IntelliNewz
At IntelliNewz, Dr. Siddiqui serves as Founder, Chief Medical Editor, and Lead Clinical Validator. Every article published is:
Evidence-based
• Clinically verified
• Technology-grounded
• Free from commercial bias
• Designed for real-world patient and physician decision-making
Through his writing, Dr. Siddiqui shares practical health intelligence, early warning signs, and preventive strategies that readers can trust — grounded in decades of frontline medical practice.
Contact:
powerofprevention@outlook.com
📌 Disclaimer: The content on IntelliNewz is intended for educational purposes only and does not replace personalized medical consultation. For individual health concerns, please consult your physician.