Learn the key symptoms of neural tube defects during pregnancy, including abnormal AFP levels, ultrasound markers, and fetal movement changes. Discover early warning signs, risk factors, and how prenatal screening helps ensure timely diagnosis.
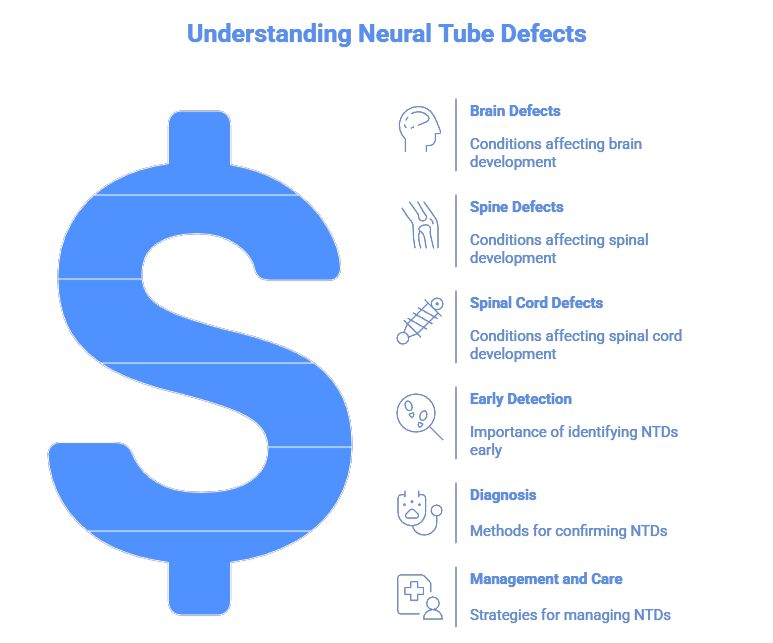
Neural tube defects (NTDs) are serious birth abnormalities affecting the brain, spine, or spinal cord. They occur very early in pregnancy—often before most women even know they are expecting. Because of this, understanding the symptoms of neural tube defects during pregnancy is essential for early detection and proper medical care.
This guide explains the warning signs, diagnostic markers, risk factors, and when to consult a healthcare provider.
What Are Neural Tube Defects?
NTDs develop when the neural tube fails to close properly during the first 4 weeks of pregnancy.
The most common types include:
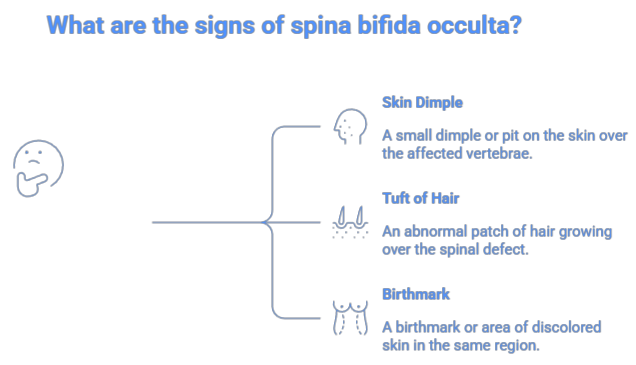
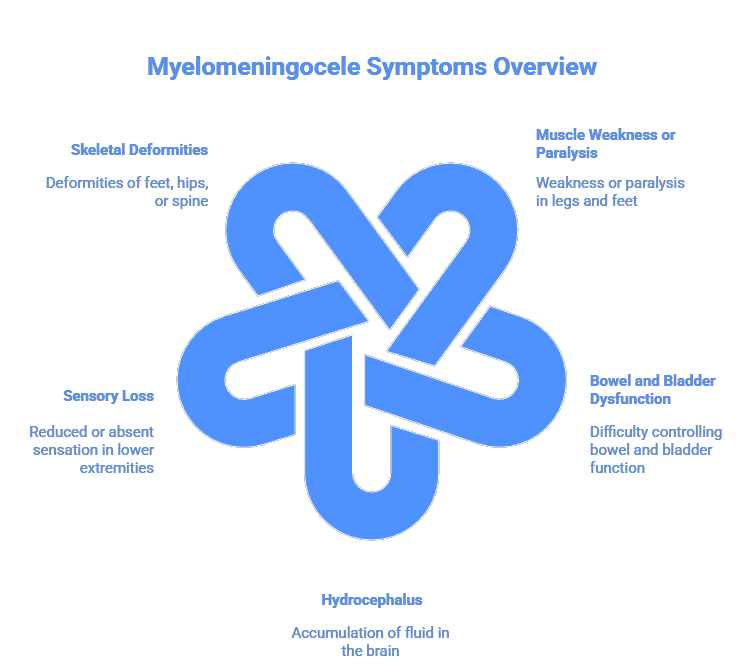
- Spina bifida – incomplete closure of the spinal column
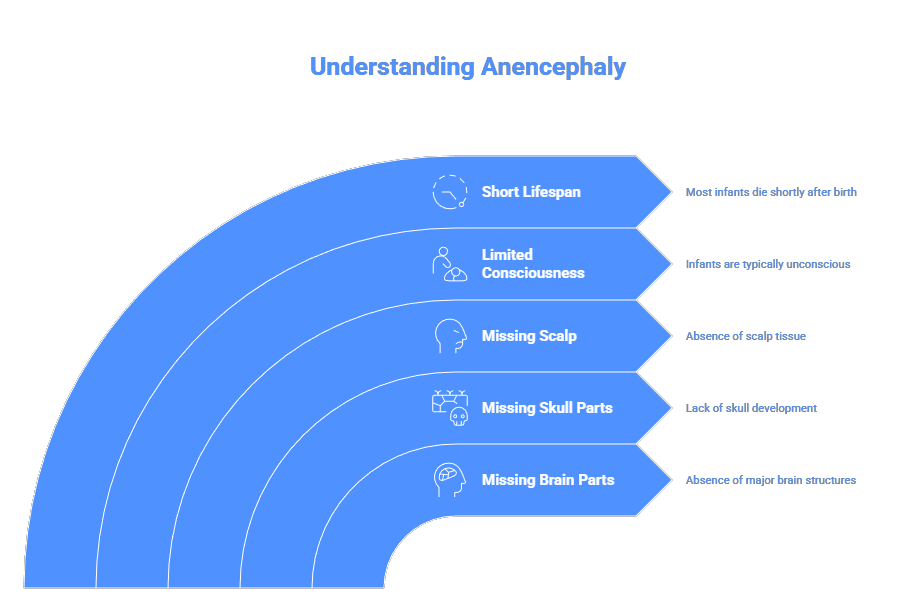
- Anencephaly – absence of major parts of the brain and skull
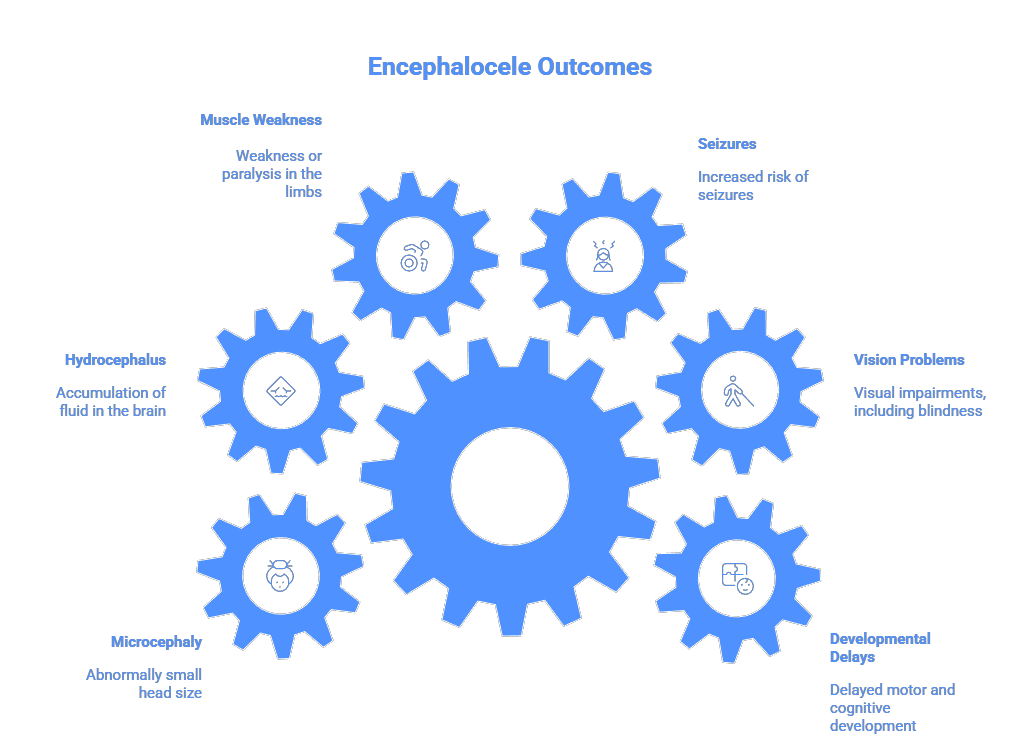
- Encephalocele – protrusion of brain tissue through the skull
Most symptoms appear through tests and scans, not through physical symptoms in the mother.
Symptoms of Neural Tube Defects During Pregnancy
While many NTDs do not cause noticeable symptoms for the mother, certain medical signs and screening results can indicate a potential problem.
1. Abnormal Maternal Serum AFP Levels (16–18 Weeks)
One of the most important early indicators is the maternal serum alpha-fetoprotein (MSAFP) test.
What the results can indicate:
- High AFP levels → possible open spina bifida
- Low AFP levels → may suggest anencephaly or other developmental issues
This test is usually performed between 15–20 weeks of pregnancy.
2. Ultrasound Abnormalities at the 18–20 Week Anatomy Scan
A detailed mid-pregnancy ultrasound can reveal physical signs of NTDs.
Potential ultrasound findings:
- Open spinal defects
- Absence of skull or brain tissue (anencephaly)
- Bulging sac on the skull (encephalocele)
- “Lemon sign” – inward curvature of the skull associated with spina bifida
- “Banana sign” – abnormal cerebellum shape
- Fluid buildup in the brain (ventriculomegaly)
This scan is the most reliable way to detect NTD symptoms.
3. Excess Amniotic Fluid (Polyhydramnios)
Some NTDs affect the baby’s ability to swallow amniotic fluid.
Possible symptoms:
- Unusually high amniotic fluid levels detected during scans
This is often linked to severe defects like anencephaly.
4. Reduced or Minimal Fetal Movement
In later stages of pregnancy, some severe NTDs involving the brain or upper spine can cause:
- Very weak or reduced fetal movement
- No movement in extreme cases
This symptom is less common with mild NTDs.
5. Abnormal Results in Detailed Fetal Imaging (MRI)
If ultrasound suggests abnormalities, doctors may order an MRI to confirm symptoms.
MRI may reveal:
- Spinal openings
- Protruding sacs of fluid or tissue
- Abnormal brain development
- Skull malformations
6. Signs Appearing After Birth
Although not prenatal, some symptoms are only clearly noticeable after delivery:
- Leg weakness or paralysis
- Bladder or bowel difficulties
- Visible spinal sac (with severe spina bifida)
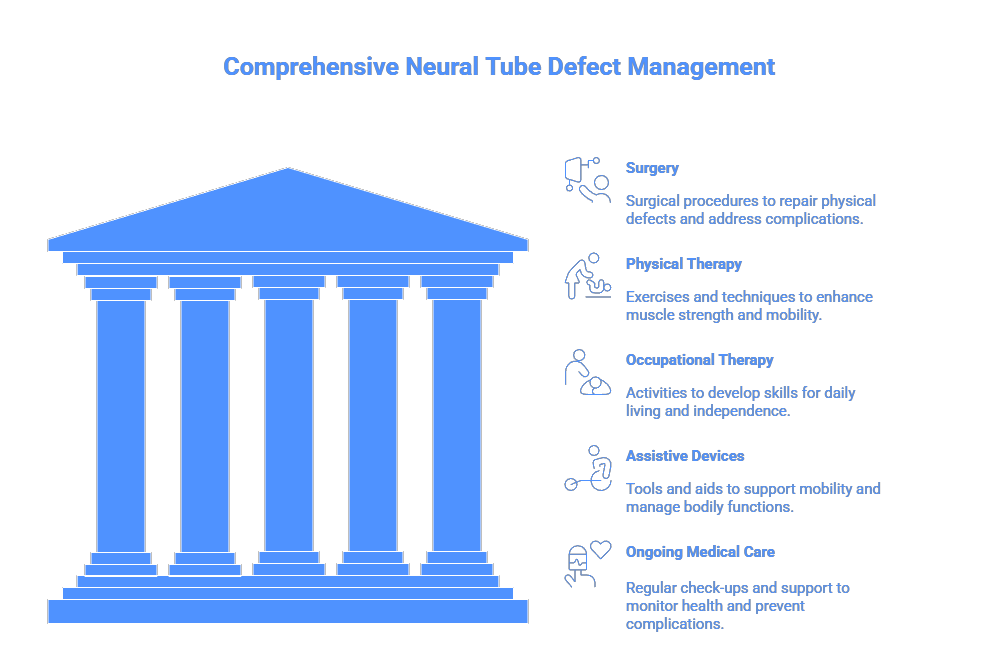
Early detection during pregnancy helps doctors plan appropriate delivery and immediate newborn care.
Do Neural Tube Defects Cause Symptoms in the Mother?
Generally, no.
Most mothers do not experience pain, discomfort, or physical symptoms related to neural tube defects.
NTDs are almost always detected through:
- Blood tests
- Ultrasound scans
- Amniocentesis
- Fetal MRI
Risk Factors for Neural Tube Defects
Understanding risk factors can help expectant mothers take preventive steps.
Higher risk is associated with:
- Low folic acid intake
- Diabetes (poorly controlled)
- Obesity
- Certain anti-seizure medications
- High fever or heat exposure early in pregnancy
- Family history of NTDs
How Neural Tube Defects Are Diagnosed
Doctors use a combination of:
Screening Tests
- Maternal serum AFP
- Quadruple screen
Diagnostic Tests
- Targeted second-trimester ultrasound
- Amniocentesis (AFP & acetylcholinesterase testing)
- Fetal MRI
These tools help determine the type and severity of the defect.
When to See a Doctor
Seek medical advice if:
- Your blood test shows abnormal AFP levels
- Your ultrasound indicates structural abnormalities
- You have a history of neural tube defects
- You plan to conceive and need folic acid guidance
Early prenatal care is essential for healthy fetal development.
Final Thoughts
Recognizing the symptoms of neural tube defects during pregnancy allows for early diagnosis, better planning, and a higher chance of positive outcomes. While mothers may not feel symptoms themselves, routine screening and imaging provide clear signs early on.
Early Signs of Neural Tube Defects in Pregnancy
While many neural tube defects show no obvious signs during early pregnancy, certain symptoms and test results can signal possible issues.
1. Abnormal Maternal Serum AFP Levels (16–18 Weeks)
One of the earliest and most common indicators is an abnormal result in the maternal serum alpha-fetoprotein (MSAFP) test.
- High AFP levels may indicate spina bifida.
- Low AFP levels may signal anencephaly or other chromosomal issues.
When it’s checked:
Usually between 15–20 weeks of pregnancy.
2. Findings on the 18–20 Week Ultrasound (Anatomy Scan)
A detailed mid-pregnancy ultrasound can reveal structural abnormalities. Possible ultrasound signs include:
- Open spinal defects
- Absence of brain/skull (anencephaly)
- Bulging sac on the skull (encephalocele)
- Lemon sign (shape of baby’s head) – associated with spina bifida
- Banana sign (curved cerebellum) – another spina bifida marker
- Fluid buildup or ventriculomegaly
This scan is the most reliable tool for detecting NTDs.
3. Excess Amniotic Fluid (Polyhydramnios)
Some neural tube defects can cause the baby to have difficulty swallowing amniotic fluid.
Possible sign:
- Excessive amniotic fluid detected during an ultrasound
This can indicate a severe NTD such as anencephaly.
4. Reduced Fetal Movement (In Severe Cases)
While not common in mild NTDs, severe brain or spinal defects may cause:
- Very little or no fetal movement
This usually appears later in pregnancy and is a warning sign for serious abnormalities.
5. Imaging Signs on Fetal MRI
If doctors suspect an NTD on ultrasound, they may recommend an MRI. Signs may include:
- Spinal gaps
- Brain protrusions
- Abnormal brain development
MRI provides better visualization of the spine and brain structure.
Risk Factors for Neural Tube Defects
While NTDs can occur in any pregnancy, certain factors increase the risk:
- Low folic acid intake before and during early pregnancy
- Family history of NTDs
- Pre-existing diabetes
- Obesity
- Anti-seizure medications (e.g., valproic acid)
- High fever or hyperthermia in early pregnancy
How Neural Tube Defects Are Diagnosed
Diagnosis usually includes:
1. Screening Tests
- MSAFP test
- Quadruple screen
2. Diagnostic Tests
- Targeted second-trimester ultrasound
- Amniocentesis – checks AFP and acetylcholinesterase levels
- Fetal MRI for detailed brain/spine imaging
Can Neural Tube Defects Be Prevented?
Not all NTDs can be prevented, but risk decreases significantly with:
Folic Acid
- 400–800 mcg/day before conception
- 4 mg/day for women with a previous NTD-affected pregnancy (under medical guidance)
Foods rich in folate include leafy greens, peas, citrus fruits, fortified cereals, and legumes.
When Should You Seek Medical Advice?
Consult your doctor if:
- Your AFP levels are abnormal
- Your ultrasound shows spinal or brain irregularities
- You have a family history of NTDs
- You are planning pregnancy and need folic acid guidance
Early detection helps doctors plan appropriate monitoring, delivery options, and newborn care.
************************************************************************
************************************************************************
Disclaimer:
Dr. Mohammed Abdul Azeem Siddiqui, MBBS
Registered Medical Practitioner (Reg. No. 39739)
With over 30 years of dedicated clinical experience, Dr. Siddiqui has built his career around one clear mission: making quality healthcare affordable, preventive, and accessible.
He is deeply passionate about:
- Early disease diagnosis – empowering patients with timely detection and reducing complications.
- Preventive healthcare – guiding individuals and families towards healthier, longer lives through lifestyle interventions and screenings.
- Affordable treatments – ensuring cost-effective, evidence-based medical solutions that reach people from all walks of life.
Through his blog, Dr. Siddiqui shares practical health insights, early warning signs, and preventive strategies that readers can trust. Every article is rooted in evidence-based medicine and enriched by decades of hands-on clinical practice.
Contact us on: powerofprevention@outlook.com
📌 Disclaimer: The content in this blog is for educational purposes only and should not replace personalized medical consultation. For specific health concerns, please consult your physician.
Dr. Mohammed Abdul Azeem Siddiqui, MBBS, M.Tech (Biomedical Engineering – VIT, Vellore)
Registered Medical Practitioner – Reg. No. 39739
Physician • Clinical Engineer • Preventive Diagnostics Specialist
Dr. Mohammed Abdul Azeem Siddiqui is a physician–engineer with over 30 years of dedicated clinical and biomedical engineering experience, committed to transforming modern healthcare from late-stage disease treatment to early detection, preventive intelligence, and affordable medical care.
He holds an MBBS degree in Medicine and an M.Tech in Biomedical Engineering from VIT University, Vellore, equipping him with rare dual expertise in clinical medicine, laboratory diagnostics, and medical device engineering. This allows him to translate complex laboratory data into precise, actionable preventive strategies.
Clinical Mission
Dr. Siddiqui’s professional mission centers on three core pillars:
Early Disease Detection
Identifying hidden biomarker abnormalities that signal chronic disease years before symptoms appear — reducing complications, hospitalizations, and long-term disability.
Preventive Healthcare
Guiding individuals and families toward longer, healthier lives through structured screenings, lifestyle intervention frameworks, and predictive diagnostic interpretation.
Affordable Evidence-Based Treatment
Delivering cost-effective, scientifically validated care accessible to people from all socioeconomic backgrounds.
Clinical & Technical Expertise
Across three decades of continuous practice, Dr. Siddiqui has worked extensively with:
Advanced laboratory analyzers and automation platforms
• Cardiac, metabolic, renal, hepatic, endocrine, and inflammatory biomarker systems
• Preventive screening and early organ damage detection frameworks
• Clinical escalation pathways and diagnostic decision-support models
• Medical device validation, calibration, compliance, and patient safety standards
He is recognized for identifying subclinical biomarker shifts that predict cardiovascular disease, diabetes, fatty liver, kidney disease, autoimmune inflammation, neurodegeneration, and accelerated biological aging long before conventional diagnosis.
Role at IntelliNewz
At IntelliNewz, Dr. Siddiqui serves as Founder, Chief Medical Editor, and Lead Clinical Validator. Every article published is:
Evidence-based
• Clinically verified
• Technology-grounded
• Free from commercial bias
• Designed for real-world patient and physician decision-making
Through his writing, Dr. Siddiqui shares practical health intelligence, early warning signs, and preventive strategies that readers can trust — grounded in decades of frontline medical practice.
Contact:
powerofprevention@outlook.com
📌 Disclaimer: The content on IntelliNewz is intended for educational purposes only and does not replace personalized medical consultation. For individual health concerns, please consult your physician.