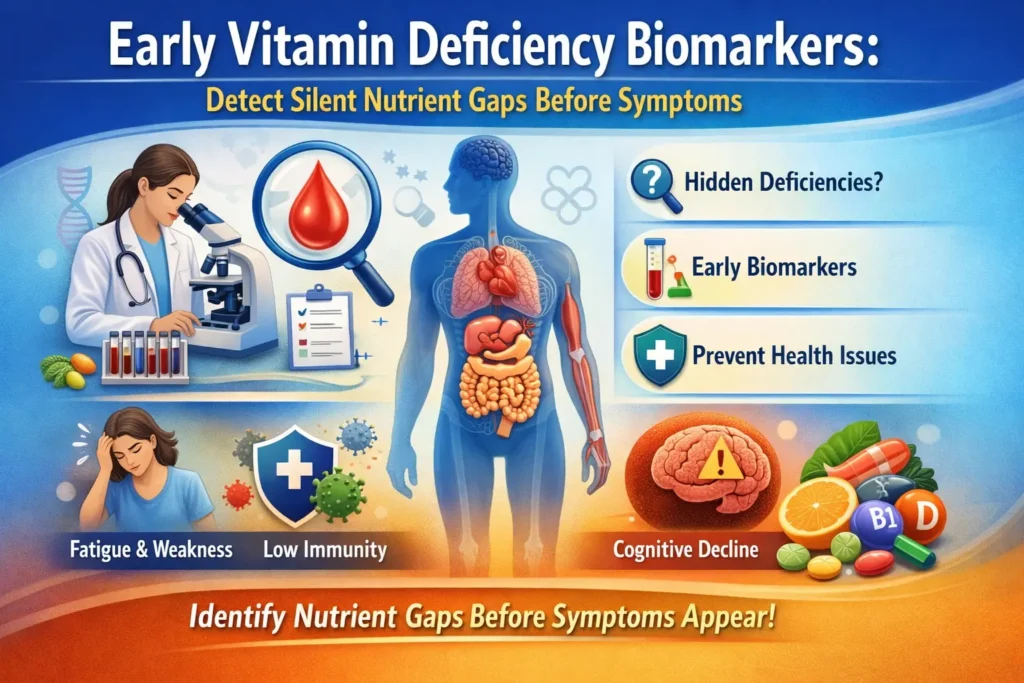
Vitamin deficiencies often develop silently, long before obvious symptoms appear. Hidden biomarkers in blood and urine can reveal early nutrient gaps, helping you prevent chronic disease, maintain energy, and optimize health.
At IntelliNewz, Dr. Azeem Siddiqui guides readers on understanding these biomarkers and taking preventive action. (NIH – Vitamin D)
1. What Are Early Vitamin Deficiency Biomarkers?
Biomarkers are measurable molecules in the body that indicate physiological changes. For vitamins, these markers can show deficiencies before clinical symptoms appear. Detecting them early allows interventions like diet changes, supplementation, or lifestyle adjustments.
Common Biomarkers:
- Vitamin D: 25-hydroxyvitamin D levels in serum. Low levels can affect bone, immunity, and heart health. (Mayo Clinic)
- Vitamin B12: Serum B12, methylmalonic acid (MMA), homocysteine. Early deficiency may cause fatigue, neuropathy, or cognitive changes. (Cleveland Clinic)
- Folate (Vitamin B9): Serum folate and RBC folate. Low levels impact DNA synthesis and red blood cell formation.
- Vitamin A: Serum retinol. Early deficiency affects vision, immunity, and skin health.
- Vitamin K: Prothrombin time or undercarboxylated osteocalcin. Low levels may impair bone health and blood clotting.
2. Clinical Cases Illustrating Early Vitamin Deficiency
| Vitamin | Clinical Case | Early Biomarker Detected | Outcome | Reference |
|---|---|---|---|---|
| Vitamin D | 34-year-old woman with chronic fatigue and mild bone pain | 25(OH)D = 15 ng/mL | Supplementation and lifestyle changes improved energy and normalized bone markers within 3 months | NCBI |
| Vitamin B12 | 45-year-old man with tingling in fingers and mild memory issues | Serum B12 = 180 pg/mL, MMA elevated | Vitamin B12 injections corrected levels; neuropathy symptoms improved within 6 weeks | NCBI |
| Folate (B9) | 29-year-old pregnant woman with normal CBC, mild fatigue | Serum folate = 3 ng/mL | Folate supplementation prevented neural tube defects risk and anemia | NCBI |
| Vitamin A | 6-year-old child with night vision difficulties | Serum retinol = 18 µg/dL | Vitamin A supplementation restored night vision within weeks | WHO |
| Vitamin K | 65-year-old male with prolonged clotting time after minor injury | Prothrombin time = 16 sec | Vitamin K supplementation corrected coagulation, reduced bleeding risk | PubMed |
3. Why Early Detection Matters
- Prevent Chronic Disease: Deficiencies contribute to osteoporosis, anemia, cardiovascular disease, and immune dysfunction (WHO)
- Optimize Energy & Performance: Early detection helps maintain vitality, brain function, and metabolism
- Guided Supplementation: Avoids over-supplementation or imbalances
4. How to Read Your Vitamin Biomarker Report
- Identify the vitamin category: Check which biomarkers are listed
- Compare with reference range: Values outside normal ranges indicate deficiency
- Look for patterns: Multiple deficiencies may indicate malabsorption or diet insufficiency
- Take action: Adjust diet, supplement responsibly, and repeat testing as recommended
5. Preventive Actions to Correct Early Deficiencies
- Vitamin D: Sun exposure, fatty fish, fortified foods, supplements if low
- Vitamin B12: Animal products, fortified cereals, injections if absorption issues
- Folate: Leafy greens, legumes, fortified grains, supplementation during pregnancy
- Vitamin A: Carrots, sweet potatoes, liver, supplements only if needed
- Vitamin K: Leafy greens, broccoli, fermented foods, monitor anticoagulants
6. FAQs – Early Vitamin Deficiency Biomarkers
Q1: Can I detect deficiencies before symptoms appear?
Yes. Blood and urine biomarkers often reveal nutrient gaps months or years before clinical symptoms (NIH)
Q2: How often should I test my vitamin biomarkers?
High-risk adults or those with chronic conditions should test annually or as advised by a physician
Q3: Can supplementation correct deficiencies?
Yes, when guided by lab results. Over-supplementation can be harmful, so follow a personalized plan
Early vitamin deficiency biomarkers are powerful tools for preventive health. Detecting silent deficiencies lets you maintain energy, immunity, and overall wellness.
At IntelliNewz, Dr. Azeem Siddiqui emphasizes regular testing, evidence-based supplementation, and personalized nutrition to optimize health and prevent chronic disease.
Section 1: Patient Demographics & Risk Factors
Q1: Age, gender, and ethnicity of the patient?
A: Vitamin D deficiency can occur at any age. Darker skin pigmentation reduces UVB-mediated synthesis. Older adults (>60) are at higher risk due to decreased cutaneous production. Gender differences are minor, though postmenopausal women are more susceptible due to bone loss.
Q2: Occupation (indoor/outdoor, sunlight exposure)?
A: Indoor workers, night shift employees, and office-bound individuals often have low sun exposure, increasing risk.
Q3: Geographic location and seasonality affecting UVB exposure?
A: Latitude >35° reduces winter UVB exposure. Seasonal variation may require higher supplementation in winter.
Q4: Skin pigmentation (fair, medium, dark)?
A: Darker skin requires longer UVB exposure to produce adequate vitamin D due to higher melanin content.
Q5: Body mass index (BMI) and obesity status?
A: Obese patients may have lower circulating 25(OH)D due to sequestration in adipose tissue; higher supplementation may be needed.
Q6: History of malabsorption syndromes (celiac, Crohn’s, bariatric surgery)?
A: Malabsorption significantly reduces vitamin D absorption; oral doses may be insufficient, and monitoring is essential.
Q7: Chronic liver or kidney disease?
A: Liver disease impairs 25-hydroxylation; kidney disease reduces conversion to active 1,25(OH)2D, requiring active analogues in severe cases.
Q8: Medications affecting vitamin D metabolism (e.g., anticonvulsants, glucocorticoids)?
A: Anticonvulsants (phenytoin, carbamazepine) increase catabolism. Chronic steroids reduce calcium absorption and vitamin D levels.
Q9: Lifestyle factors: dietary intake of vitamin D, supplementation history?
A: Dietary sources alone often insufficient; history of noncompliance or inadequate supplementation increases deficiency risk.
Q10: History of previous fractures or osteoporosis?
A: Positive history signals long-standing deficiency or secondary bone disease.
Section 2: Clinical Presentation
Q11: Symptoms of deficiency: fatigue, myalgia, bone pain, mood disturbances?
A: Early deficiency may be asymptomatic. Fatigue, muscle weakness, and diffuse bone pain are common subtle presentations.
Q12: Signs: proximal muscle weakness, gait abnormalities, skeletal deformities?
A: Proximal myopathy, waddling gait, and bone deformities (rickets in children) may appear in advanced cases.
Q13: History of recurrent infections (immune dysfunction)?
A: Vitamin D modulates innate immunity; deficiency may increase susceptibility to respiratory infections.
Q14: Dental issues: enamel hypoplasia or delayed eruption in children?
A: Severe early-life deficiency can impair dental development and enamel formation.
Q15: Any history of rickets in childhood or osteomalacia in adults?
A: Past rickets or adult osteomalacia is a strong predictor of ongoing or recurrent deficiency.
Section 3: Laboratory Assessment
Q16: Serum 25-hydroxyvitamin D [25(OH)D] level: current and past trends?
A: Gold standard marker. <20 ng/mL = deficiency, 20–30 ng/mL = insufficiency, >30 ng/mL = sufficient.
Q17: Serum 1,25-dihydroxyvitamin D [1,25(OH)2D] in special cases?
A: Not routinely measured; useful in renal disease or suspected resistance syndromes.
Q18: Serum calcium, phosphate, and alkaline phosphatase levels?
A: Low vitamin D may cause secondary hyperparathyroidism, low-normal calcium, low phosphate, and elevated alkaline phosphatase.
Q19: Parathyroid hormone (PTH) levels – evidence of secondary hyperparathyroidism?
A: PTH rises in response to chronic deficiency to maintain calcium homeostasis.
Q20: Vitamin D binding protein levels, if tested?
A: Rarely measured; altered levels can affect total 25(OH)D but free levels remain functional.
Q21: Urinary calcium excretion and phosphate studies?
A: Helps identify malabsorption or renal phosphate wasting in severe cases.
Q22: Bone turnover markers (osteocalcin, P1NP, CTX)?
A: Can indicate high bone turnover due to secondary hyperparathyroidism.
Q23: Any genetic testing for vitamin D receptor polymorphisms in resistant cases?
A: Considered in rare cases of vitamin D–resistant rickets or unexplained persistent deficiency.
Section 4: Imaging & Functional Assessment
Q24: Bone mineral density (DEXA scan) results: lumbar spine, hip, forearm?
A: DEXA helps quantify osteoporosis risk; low T-score (<-2.5) may indicate chronic deficiency effects.
Q25: X-ray evidence of osteomalacia or rickets?
A: Adults: Looser zones; children: metaphyseal widening, cupping, fraying.
Q26: MRI/CT findings if musculoskeletal pain is unexplained?
A: Can detect stress fractures, pseudofractures, and bone marrow edema.
Q27: Functional assessment: muscle strength testing, gait evaluation?
A: Weakness in hip flexors, difficulty rising from chair, impaired balance — common in elderly with deficiency.
Section 5: Comorbidities & Complications
Q28: Presence of osteoporosis, fractures, or falls history?
A: Strong correlation with chronic deficiency; supplementation plus weight-bearing exercise reduces risk.
Q29: Autoimmune conditions potentially influenced by vitamin D?
A: MS, type 1 diabetes, SLE show association; supplementation may modulate immune response.
Q30: Cardiovascular risk profile: hypertension, diabetes, dyslipidemia?
A: Low vitamin D linked to increased CV risk; correction may improve endothelial function modestly.
Q31: Chronic pain syndromes or fibromyalgia?
A: Often coexists; correcting deficiency can alleviate musculoskeletal pain in some patients.
Q32: Cognitive or mood disorders (depression, seasonal affective disorder)?
A: Deficiency is associated with fatigue, depression, and impaired cognitive function; supplementation may help.
Q33: Malignancy history: colorectal, breast, prostate (Vitamin D status relevance)?
A: Observational studies suggest low vitamin D may increase risk; evidence for supplementation in prevention is limited but safe.
Section 6: Therapeutic Interventions
Q34: Previous vitamin D supplementation: dose, duration, adherence?
A: Oral D3 preferred; weekly/monthly dosing can improve adherence.
Q35: Response to supplementation: improvement in labs and symptoms?
A: Levels usually normalize in 8–12 weeks; muscle strength and fatigue improve within weeks.
Q36: Calcium supplementation history and dietary calcium intake?
A: Adequate calcium intake is essential for optimal bone health alongside vitamin D.
Q37: Choice of vitamin D formulation (D2 vs D3, oral vs injectable)?
A: D3 is more potent than D2; injectable forms reserved for malabsorption or noncompliance.
Q38: Any history of toxicity or hypercalcemia with prior therapy?
A: Rare; usually occurs with excessive high-dose therapy (>10,000 IU/day for months).
Q39: Sunlight exposure recommendations provided to patient?
A: Safe exposure: 10–30 min, 2–3 times/week depending on skin type and latitude.
Q40: Weight loss, exercise, or dietary modification interventions advised?
A: Weight reduction in obesity improves bioavailability; resistance exercise improves bone density.
Section 7: Follow-Up & Monitoring
Q41: Frequency of repeat serum 25(OH)D measurement?
A: 8–12 weeks after therapy initiation, then every 6–12 months once stable.
Q42: Monitoring of calcium, phosphate, PTH, and alkaline phosphatase?
A: Especially in high-dose therapy or renal disease; detect secondary effects early.
Q43: Bone mineral density reassessment interval?
A: Every 1–2 years in high-risk adults or postmenopausal women.
Q44: Tracking functional outcomes: muscle strength, gait, fall risk?
A: Assess quarterly in elderly or symptomatic patients.
Q45: Preventive education provided: safe sun exposure, dietary sources?
A: Yes; fortified foods, oily fish, eggs, mushrooms, and supplements if needed.
Section 8: Special Populations
Q46: Pregnant or lactating women: vitamin D status and supplementation strategy?
A: 600–2000 IU/day safe; deficiency increases risk of neonatal hypocalcemia and low birth weight.
Q47: Children and adolescents: growth, skeletal development, supplementation?
A: 400–600 IU/day recommended; monitor for rickets and growth delay.
Q48: Elderly: fall prevention, fracture risk, vitamin D dosing adjustments?
A: 800–2000 IU/day; combine with calcium and exercise; monitor for kidney function.
Q49: Patients with chronic kidney disease: calcitriol or analogues usage?
A: Use active forms (calcitriol, alfacalcidol) if 1α-hydroxylation impaired; monitor calcium and phosphate.
Q50: Bariatric surgery patients: high-risk for deficiency — monitoring and supplementation protocols?
A: Lifelong monitoring required; high-dose D3 (3000–5000 IU/day) or injectable may be necessary; combine with calcium and multivitamins.

Dr. Mohammed Abdul Azeem Siddiqui, MBBS, M.Tech (Biomedical Engineering – VIT, Vellore)
Registered Medical Practitioner – Reg. No. 39739
Physician • Clinical Engineer • Preventive Diagnostics Specialist
Dr. Mohammed Abdul Azeem Siddiqui is a physician–engineer with over 30 years of dedicated clinical and biomedical engineering experience, committed to transforming modern healthcare from late-stage disease treatment to early detection, preventive intelligence, and affordable medical care.
He holds an MBBS degree in Medicine and an M.Tech in Biomedical Engineering from VIT University, Vellore, equipping him with rare dual expertise in clinical medicine, laboratory diagnostics, and medical device engineering. This allows him to translate complex laboratory data into precise, actionable preventive strategies.
Clinical Mission
Dr. Siddiqui’s professional mission centers on three core pillars:
Early Disease Detection
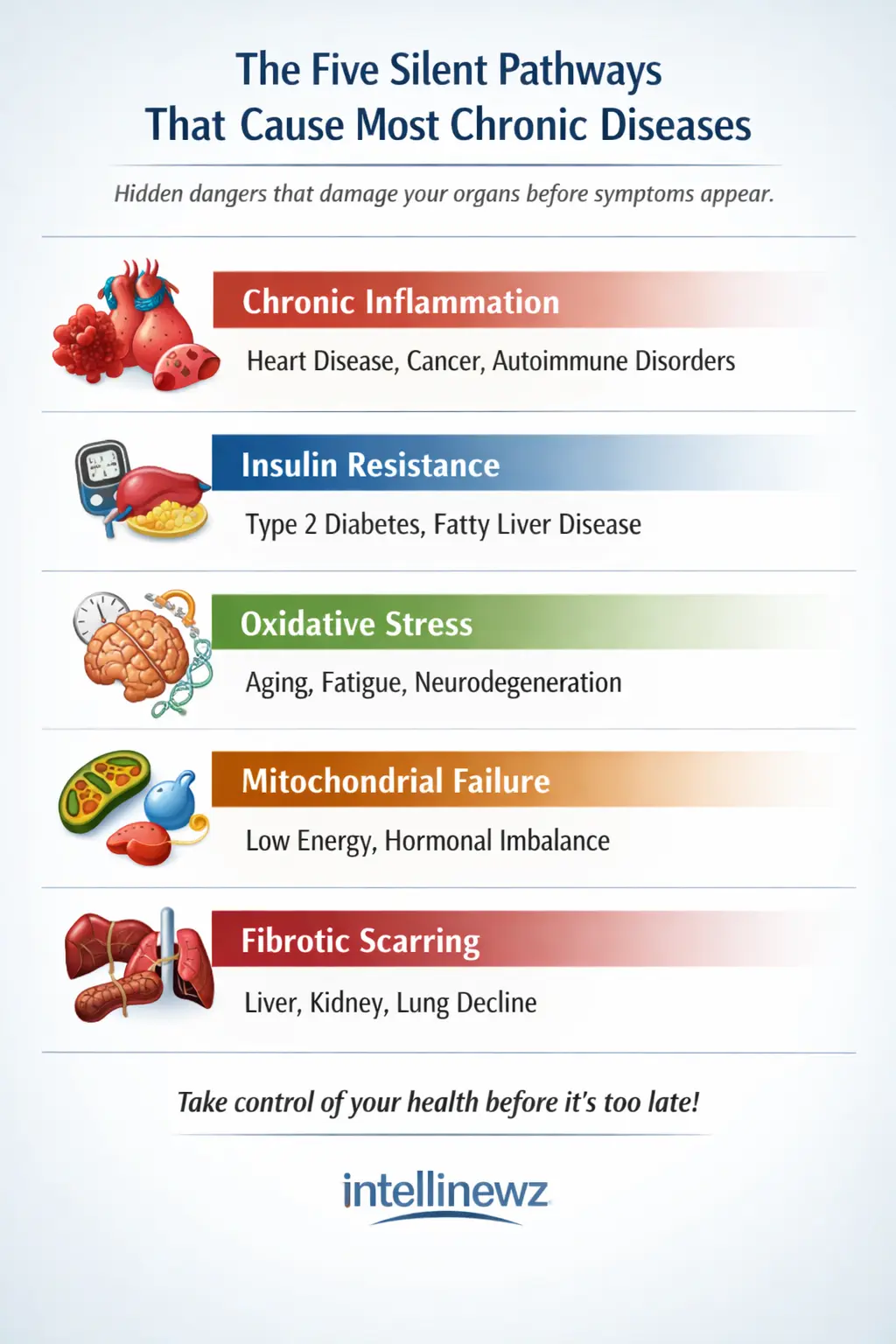
Identifying hidden biomarker abnormalities that signal chronic disease years before symptoms appear — reducing complications, hospitalizations, and long-term disability.
Preventive Healthcare
Guiding individuals and families toward longer, healthier lives through structured screenings, lifestyle intervention frameworks, and predictive diagnostic interpretation.
Affordable Evidence-Based Treatment
Delivering cost-effective, scientifically validated care accessible to people from all socioeconomic backgrounds.
Clinical & Technical Expertise
Across three decades of continuous practice, Dr. Siddiqui has worked extensively with:
Advanced laboratory analyzers and automation platforms
• Cardiac, metabolic, renal, hepatic, endocrine, and inflammatory biomarker systems
• Preventive screening and early organ damage detection frameworks
• Clinical escalation pathways and diagnostic decision-support models
• Medical device validation, calibration, compliance, and patient safety standards
He is recognized for identifying subclinical biomarker shifts that predict cardiovascular disease, diabetes, fatty liver, kidney disease, autoimmune inflammation, neurodegeneration, and accelerated biological aging long before conventional diagnosis.
Role at IntelliNewz
At IntelliNewz, Dr. Siddiqui serves as Founder, Chief Medical Editor, and Lead Clinical Validator. Every article published is:
Evidence-based
• Clinically verified
• Technology-grounded
• Free from commercial bias
• Designed for real-world patient and physician decision-making
Through his writing, Dr. Siddiqui shares practical health intelligence, early warning signs, and preventive strategies that readers can trust — grounded in decades of frontline medical practice.
Contact:
powerofprevention@outlook.com
📌 Disclaimer: The content on IntelliNewz is intended for educational purposes only and does not replace personalized medical consultation. For individual health concerns, please consult your physician.