CRISPR for Detecting Endometrial Cancer Early
Endometrial cancer — cancer of the uterine lining — is the most common gynecologic cancer in women worldwide and the fourth most common cancer among women in the United States. According to global cancer data, more than 417,000 women are diagnosed every year, with rising incidence in North America, Europe, and parts of Asia due to obesity, diabetes, and hormonal disorders.
While early-stage endometrial cancer is often highly treatable, late diagnosis dramatically reduces survival rates and increases the need for aggressive surgery, radiation, or chemotherapy.
“CRISPR is transforming endometriosis from a painful mystery into a genetically manageable disease—while also helping protect women from future cancer risk through personalized, precision care.”
— Dr. Mohammed Abdul Azeem Siddiqui
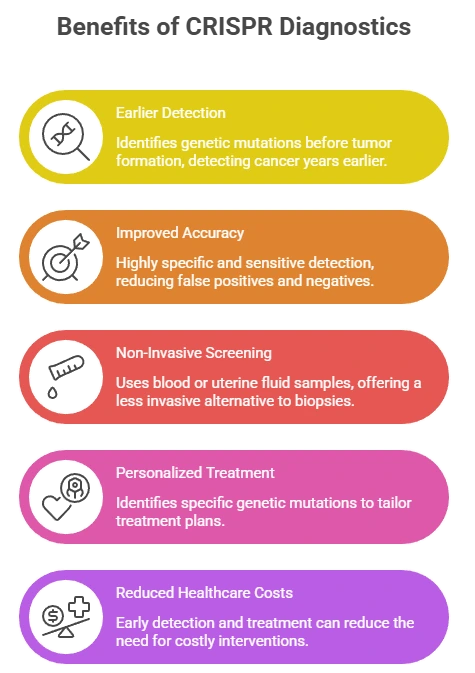
CRISPR-based diagnostics are now offering a breakthrough in molecular-level early detection, allowing women to identify cancer risk before symptoms appear or the disease spreads.
Why Early Detection Matters
Endometrial cancer symptoms such as:
- Abnormal vaginal bleeding
- Pelvic pain or pressure
- Unusual discharge
often appear after cancer has already progressed. Many women — especially postmenopausal or perimenopausal women — dismiss early bleeding as hormonal changes, delaying diagnosis.

CRISPR Liquid Biopsy – Technology & Science
Understand how CRISPR works, the science behind liquid biopsies, and why it can detect even single-molecule cancer mutations with high precision.
Traditional detection methods include:
- Transvaginal ultrasound
- Endometrial biopsy
- Blood tests for tumor markers
While useful, these methods do not detect microscopic genetic changes, meaning early disease can still go unnoticed.
CRISPR diagnostics fill this critical gap by detecting molecular mutations before tumors become visible on scans.
How CRISPR Detects Endometrial Cancer
CRISPR-based cancer tests work at the genetic and RNA level, identifying early cancer signals in body fluids.
Step-by-step process:
- Sample collection – blood, uterine fluid, or endometrial tissue
- DNA/RNA extraction – isolating cancer-related genetic material
- CRISPR targeting – engineered guide RNAs locate cancer mutations
- Signal detection – fluorescence or electrical signal confirms mutation
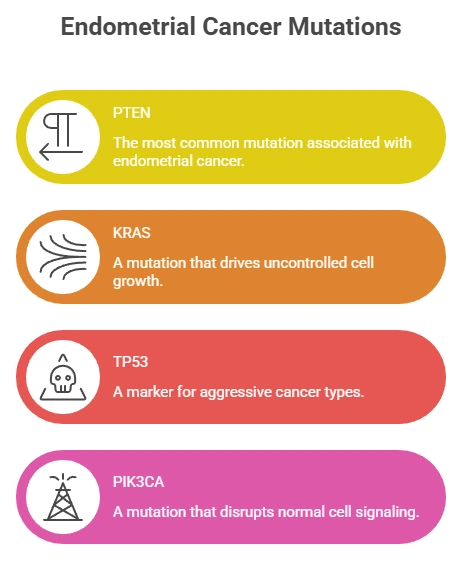
Key Genes Detected by CRISPR
- PTEN – tumor suppressor loss (very common in endometrial cancer)
- KRAS – mutation linked to uncontrolled cell growth
- TP53 – aggressive and high-risk cancers
- PIK3CA – abnormal proliferation signaling
These mutations often appear years before cancer becomes symptomatic.
Advantages of CRISPR Testing
| Feature | Traditional Methods | CRISPR-Based Detection |
|---|---|---|
| Sensitivity | Moderate | Extremely high |
| Early detection | After symptoms | Pre-symptomatic |
| Invasiveness | Biopsy or imaging | Blood or fluid test |
| Precision | Limited | Targets exact mutations |
CRISPR enables non-invasive, rapid, and ultra-precise screening, especially for women at higher risk.
Who Should Consider CRISPR Screening
CRISPR testing may benefit women who:
- Are over 50 or postmenopausal
- Have a family history of endometrial, ovarian, or colorectal cancer
- Have obesity, PCOS, diabetes, or metabolic syndrome
- Experience irregular bleeding or hormone imbalance
- Carry Lynch syndrome or BRCA-related risks
- Want preventive cancer monitoring
Global & U.S. Relevance
In the United States, endometrial cancer is rising faster than any other gynecologic cancer. Minority populations, especially Black women, face higher mortality due to delayed diagnosis and unequal access to care.
CRISPR diagnostics could help:
- Enable earlier screening for underserved populations
- Reduce diagnostic delays in rural and low-income communities
- Support personalized surveillance for high-risk women
Globally, CRISPR-based blood or fluid tests could be used in low-resource healthcare systems, where biopsy and imaging access is limited.
The Future of Endometrial Cancer Care
CRISPR is transforming cancer prevention by:
- Identifying genetic risk before tumors form
- Guiding personalized monitoring and treatment
- Reducing unnecessary invasive procedures
- Increasing survival through early intervention
With further validation and regulatory approval, CRISPR diagnostics may soon become a routine part of women’s preventive healthcare.
If you’d like, I can next:
- Add FAQs + schema markup
- Create a pillar → symptoms → detection → eligibility → trust version
- Or adapt this for Google Discover / hospital websites / legal awareness pages
adapt for discover
Perfect — this topic is ideal for Google Discover. Below is your content adapted and optimized for Discover: emotionally engaging, scannable, authoritative, and written for women in the U.S. and globally.
A New CRISPR Blood Test Could Detect Endometrial Cancer Before Symptoms Appear
Endometrial cancer — cancer of the uterine lining — is now the most common gynecologic cancer in women and one of the fastest-rising cancers in the United States.
Every year, more than 417,000 women worldwide are diagnosed. In the U.S. alone, cases continue to climb, especially among women over 50, those with obesity, diabetes, PCOS, or a family history of cancer.
The biggest danger?
Most women are diagnosed only after symptoms appear.
Now, a breakthrough in genetic science may change everything.
CRISPR-based diagnostics can detect the earliest molecular signals of endometrial cancer—long before tumors are visible or symptoms begin.
This could redefine how women protect their health.
Why Endometrial Cancer Is Often Found Too Late
Early-stage endometrial cancer is highly treatable. But once it spreads, survival rates drop sharply.
The problem is that early warning signs like:
- Abnormal bleeding
- Pelvic pain
- Unusual discharge
are often mistaken for hormonal changes, menopause, or stress. By the time women seek care, cancer may already be advanced.
Traditional tools—ultrasound, biopsy, and tumor markers—cannot detect the first genetic changes that trigger cancer.
That’s where CRISPR changes the game.
How CRISPR Finds Cancer at the Genetic Level
CRISPR diagnostics don’t look for tumors.
They look for mutations that create tumors.
Using a simple blood or uterine fluid sample, CRISPR systems scan for DNA and RNA changes linked to endometrial cancer, including:
- PTEN – the most common mutation
- KRAS – drives uncontrolled growth
- TP53 – aggressive cancer marker
- PIK3CA – abnormal cell signaling
These changes can appear years before cancer is visible on scans.
Why This Could Be a Turning Point for Women’s Health
CRISPR testing offers:
| What Women Need | What CRISPR Delivers |
|---|---|
| Early detection | Pre-symptom diagnosis |
| Less invasive care | Blood or fluid test |
| Accurate results | Gene-level precision |
| Faster answers | Rapid detection |
This is especially powerful for women who are at high risk but have no symptoms yet.
Who Should Pay Attention to This Breakthrough
You may benefit from early CRISPR screening if you:
- Are postmenopausal or over 50
- Have PCOS, obesity, diabetes, or hormone imbalance
- Have a family history of endometrial, ovarian, or colorectal cancer
- Carry Lynch syndrome or inherited cancer risk
- Have irregular bleeding or fertility concerns
Why This Matters in the U.S. and Worldwide
In the United States, endometrial cancer is rising faster than any other gynecologic cancer. Black women face significantly higher death rates, largely due to delayed diagnosis and limited access to care.
CRISPR-based tests could help close that gap by enabling:
- Earlier screening in underserved communities
- Less dependence on invasive biopsies
- Personalized risk tracking for women worldwide
In low-resource countries, a simple blood-based CRISPR test could offer life-saving early detection where imaging and pathology are unavailable.
The Future: Preventing Cancer Before It Starts
While CRISPR-based diagnostics are still in the early stages of development, the potential benefits are undeniable. Ongoing research and clinical trials are focused on refining the technology, expanding the range of detectable mutations, and developing user-friendly diagnostic tools.
As CRISPR technology continues to advance, it holds the promise of transforming endometrial cancer screening and detection, ultimately leading to improved outcomes and a better quality of life for women.
CRISPR doesn’t just detect cancer—it reveals risk before disease develops.
This means:
- Earlier monitoring
- Fewer surgeries
- Higher survival
- Better quality of life
For the first time, women may be able to catch endometrial cancer before it has the chance to grow.
1. What are the very first signs of endometrial cancer I should watch for?
The earliest sign is abnormal vaginal bleeding, especially after menopause or between periods. Other early clues include watery or blood-tinged discharge, pelvic discomfort, bloating, and changes that don’t improve over time.
2. Can endometrial cancer be found before I have any symptoms?
Yes. Emerging genetic tools like CRISPR-based tests can detect cancer-related DNA and RNA changes in blood or uterine fluid before tumors form or symptoms appear, allowing much earlier monitoring and treatment.
3. How accurate is the CRISPR test for detecting endometrial cancer?
CRISPR diagnostics are highly sensitive at detecting specific cancer mutations. While still in research and early clinical use, studies show they can identify molecular changes far earlier than imaging or biopsy alone.
4. What causes the genetic mutations that lead to uterine cancer?
Mutations can develop from hormone imbalances, obesity, diabetes, chronic inflammation, inherited syndromes like Lynch, aging, and environmental factors. Over time, these changes disrupt normal cell growth and trigger uncontrolled uterine cell division.
5. Who is most at risk for endometrial cancer?
Women over 50, those who are postmenopausal, have obesity, PCOS, diabetes, or a family history of uterine or colorectal cancer are at higher risk, as are women with long-term estrogen exposure.
6. Is there a blood test that can detect endometrial cancer early?
Standard blood tests cannot reliably detect early endometrial cancer. However, CRISPR-based blood tests under development can identify genetic cancer markers, potentially offering a non-invasive way to screen before symptoms appear.
7. Can genetic screening help prevent endometrial cancer?
Genetic screening can’t stop cancer directly, but it helps identify high-risk women early. This allows closer monitoring, lifestyle changes, hormone management, and early treatment that may prevent advanced disease.
8. How is CRISPR different from a biopsy or ultrasound for cancer detection?
Ultrasound and biopsy detect visible or structural changes. CRISPR identifies microscopic genetic mutations that appear long before tumors form, making it a powerful tool for pre-symptom and precision-based cancer screening.
9. What should I do if I have abnormal bleeding but my ultrasound is normal?
You should see a gynecologist for further evaluation, including possible biopsy or genetic testing. Normal imaging does not rule out early cancer, especially if bleeding is persistent or occurs after menopause.
10. Is endometrial cancer curable if it’s found early?
Yes. When detected early, endometrial cancer has survival rates above 90 percent. Treatment is often highly effective, and early diagnosis reduces the need for aggressive therapies and improves long-term outcomes.
Dr. Mohammed Abdul Azeem Siddiqui, MBBS, M.Tech (Biomedical Engineering – VIT, Vellore)
Registered Medical Practitioner – Reg. No. 39739
Physician • Clinical Engineer • Preventive Diagnostics Specialist
Dr. Mohammed Abdul Azeem Siddiqui is a physician–engineer with over 30 years of dedicated clinical and biomedical engineering experience, committed to transforming modern healthcare from late-stage disease treatment to early detection, preventive intelligence, and affordable medical care.
He holds an MBBS degree in Medicine and an M.Tech in Biomedical Engineering from VIT University, Vellore, equipping him with rare dual expertise in clinical medicine, laboratory diagnostics, and medical device engineering. This allows him to translate complex laboratory data into precise, actionable preventive strategies.
Clinical Mission
Dr. Siddiqui’s professional mission centers on three core pillars:
Early Disease Detection
Identifying hidden biomarker abnormalities that signal chronic disease years before symptoms appear — reducing complications, hospitalizations, and long-term disability.
Preventive Healthcare
Guiding individuals and families toward longer, healthier lives through structured screenings, lifestyle intervention frameworks, and predictive diagnostic interpretation.
Affordable Evidence-Based Treatment
Delivering cost-effective, scientifically validated care accessible to people from all socioeconomic backgrounds.
Clinical & Technical Expertise
Across three decades of continuous practice, Dr. Siddiqui has worked extensively with:
Advanced laboratory analyzers and automation platforms
• Cardiac, metabolic, renal, hepatic, endocrine, and inflammatory biomarker systems
• Preventive screening and early organ damage detection frameworks
• Clinical escalation pathways and diagnostic decision-support models
• Medical device validation, calibration, compliance, and patient safety standards
He is recognized for identifying subclinical biomarker shifts that predict cardiovascular disease, diabetes, fatty liver, kidney disease, autoimmune inflammation, neurodegeneration, and accelerated biological aging long before conventional diagnosis.
Role at IntelliNewz
At IntelliNewz, Dr. Siddiqui serves as Founder, Chief Medical Editor, and Lead Clinical Validator. Every article published is:
Evidence-based
• Clinically verified
• Technology-grounded
• Free from commercial bias
• Designed for real-world patient and physician decision-making
Through his writing, Dr. Siddiqui shares practical health intelligence, early warning signs, and preventive strategies that readers can trust — grounded in decades of frontline medical practice.
Contact:
powerofprevention@outlook.com
📌 Disclaimer: The content on IntelliNewz is intended for educational purposes only and does not replace personalized medical consultation. For individual health concerns, please consult your physician.