You can sleep eight hours, eat “healthy,” and still wake up feeling exhausted.
The Silent Energy Crisis: How Mitochondrial Dysfunction Steals Your Vitality
You can sleep eight hours, eat “healthy,” and still wake up feeling exhausted. Blood tests come back normal. Doctors say everything looks fine. Yet your body feels heavy, foggy, and slow.
This experience, increasingly common in modern society, represents a fundamental disconnect between conventional medical assessment and cellular reality.
MEDICAL DISCLAIMER
This content is for educational purposes only and is not medical advice. It is not a substitute for professional medical diagnosis or treatment. Always seek the advice of your physician or qualified healthcare provider with any questions regarding a medical condition. Consult a healthcare professional before making any changes to your diet, lifestyle, or treatment plan.
You’re told you’re healthy by all measurable standards, yet you navigate your days in a persistent energy deficit, where simple tasks feel mountainous and mental clarity seems like a distant memory.
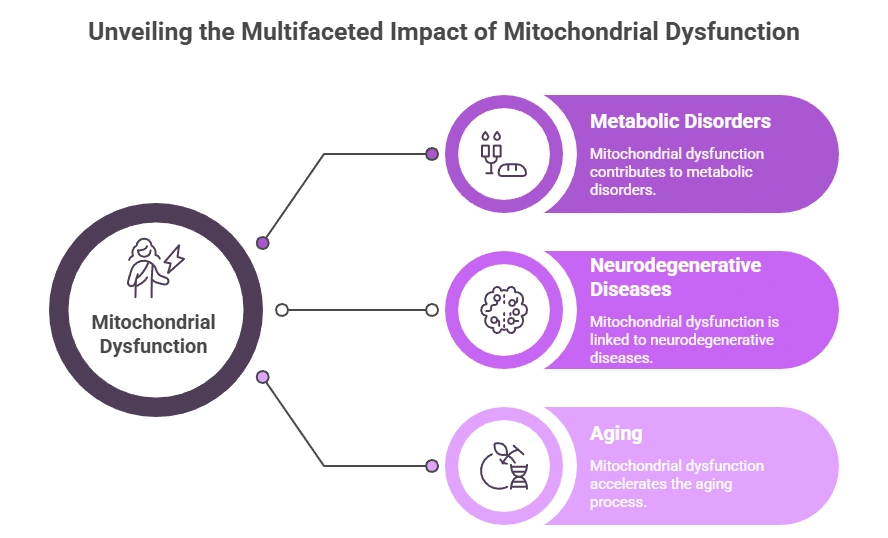
What most people never hear is this: Energy is not created by your organs. It is created inside your cells. When tiny structures called mitochondria stop working properly, your body begins to run on low power long before disease appears on scans or lab reports. This silent breakdown is now being linked to chronic fatigue, brain fog, poor recovery, mood changes, and even faster aging. The emerging science of mitochondrial health reveals that our collective exhaustion may not be a psychological failing or mere byproduct of busy lives, but a physiological crisis occurring at the microscopic level.
The good news? Mitochondria are adaptable—and when supported, they can recover. Understanding and nurturing these cellular power plants may hold the key to reclaiming the vitality that modern life systematically depletes.
What Are Mitochondria? The Unseen Power Grid of Your Body
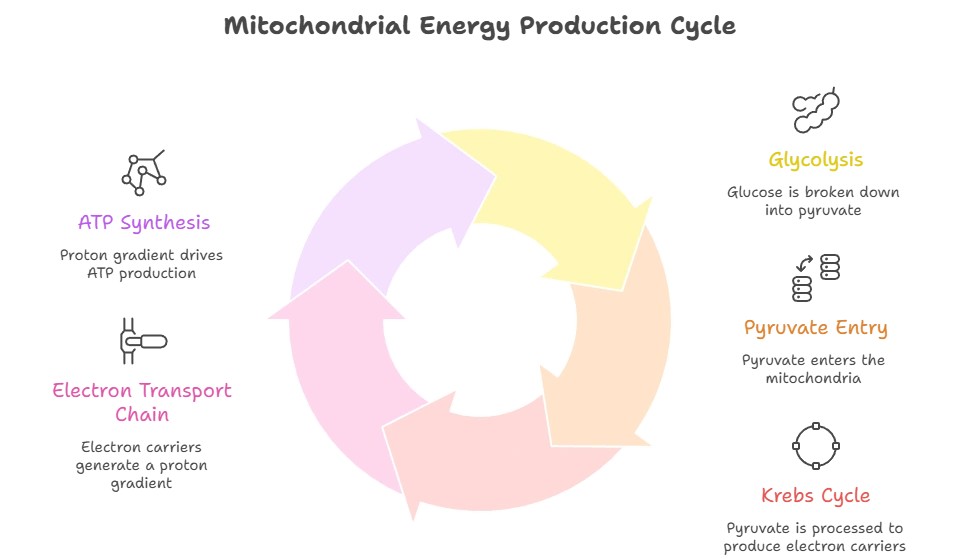
Mitochondria are microscopic, bean-shaped structures found inside nearly every cell in your body, numbering from hundreds to thousands per cell depending on energy demands. Their job is simple but vital: they convert the food you eat and the oxygen you breathe into ATP (adenosine triphosphate)—the molecule that powers every movement, thought, and heartbeat. This process, known as cellular respiration, is arguably the most important biochemical reaction sustaining human life.
If your body were a city, mitochondria would be the power stations. No electricity means no lights, no transport, no communication. Similarly, without properly functioning mitochondria, cellular processes slow, neural communication falters, muscles weaken, and detoxification pathways become sluggish. Interestingly, mitochondria have their own DNA, separate from the nucleus, suggesting an evolutionary past as independent bacteria that formed a symbiotic relationship with our cells—a partnership upon which all complex life depends.
When mitochondria are healthy, you feel alert, strong, and resilient. You recover quickly from exercise, handle stress with grace, and maintain mental clarity throughout the day. When they are damaged, overloaded, or inefficient, the entire system slows down. You might notice this not as a single dramatic symptom, but as a pervasive dragging sensation, as if you’re constantly operating at 60% capacity while the world demands 100%.
How Your Body Actually Produces Energy: Beyond Calories and Caffeine
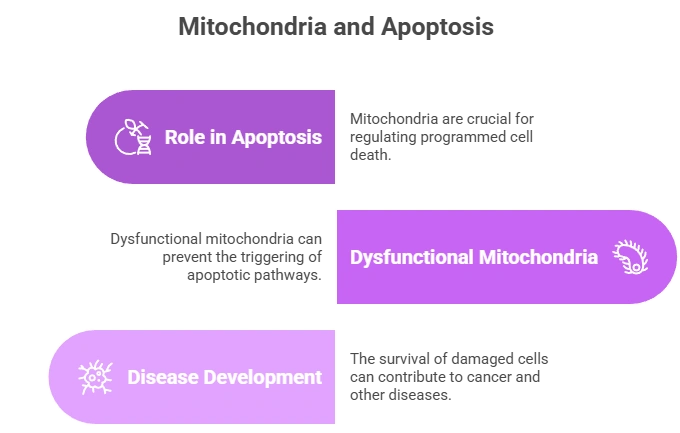
Many people believe energy comes from calories or caffeine. We’re taught that eating enough food provides energy, and that coffee gives us a boost. In reality, food is only potential energy. It must pass through complex chemical reactions inside mitochondria to become usable ATP. This transformation involves multiple steps: the Krebs cycle, electron transport chain, and oxidative phosphorylation—processes that require specific nutrients, proper oxygen utilization, and healthy mitochondrial membranes to function optimally.
If this system is blocked or inefficient, you can eat more, sleep more, and drink more coffee—yet still feel drained. The calories enter your body but fail to convert efficiently into cellular energy. Instead, they might be stored as fat or contribute to metabolic byproducts that further burden your system. This explains why two people can consume identical meals yet experience dramatically different energy levels afterward.
Caffeine does not create energy. It only forces your nervous system to ignore the fatigue signal by blocking adenosine receptors. This is akin to cutting the wires to a low-fuel warning light in your car. The problem isn’t solved; you’re just no longer aware of it. Over time, this pushes already struggling mitochondria into deeper burnout as you demand energy they cannot sustainably produce.
What Damages Mitochondria? The Perfect Storm of Modern Life
Modern life creates unprecedented challenges for these ancient energy producers. Our mitochondria evolved in a world of movement, whole foods, natural light cycles, and minimal toxins. Today, they face a constant assault that impairs their function:
1. Chronic Stress
When stress becomes constant rather than episodic, cortisol and other stress hormones remain elevated, directly interfering with mitochondrial function. Stress triggers the “survival mode” sympathetic nervous system, which diverts resources away from cellular maintenance and repair. Chronically high cortisol damages mitochondrial DNA, reduces mitochondrial density, and impairs their ability to produce ATP efficiently. The very system designed to help us survive immediate threats becomes toxic when constantly activated.
2. Blood Sugar Spikes
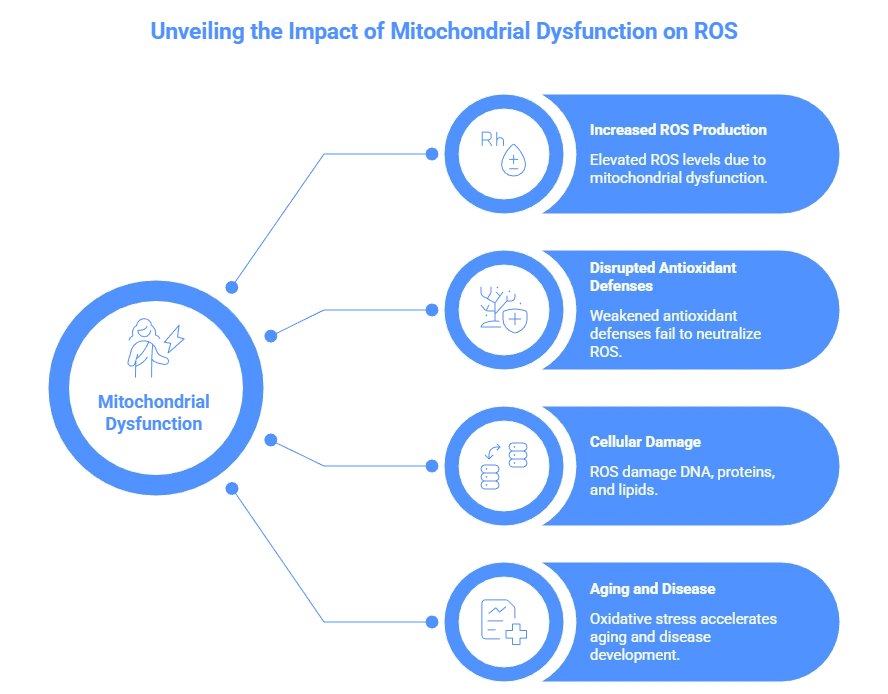
The modern diet, rich in refined carbohydrates and sugars, creates repeated glucose surges that mitochondria must process. Each spike generates free radicals—unstable molecules that damage mitochondrial membranes and DNA. Over time, this oxidative stress overwhelms antioxidant defenses, leading to mitochondrial inefficiency. Furthermore, insulin resistance, which develops from repeated sugar spikes, impairs the cell’s ability to take in glucose, starving mitochondria of their primary fuel.
3. Poor Sleep Quality and Quantity
Deep sleep, particularly slow-wave sleep, is when mitochondria undergo repair, replication, and removal of damaged components (mitophagy). Fragmented or insufficient sleep disrupts these essential maintenance processes. Research shows that just one night of poor sleep can reduce mitochondrial function in certain tissues. Chronic sleep deprivation leads to accumulated mitochondrial damage that manifests as persistent fatigue.
4. Blue Light at Night
Artificial light, particularly the blue spectrum from screens and LED lighting, suppresses melatonin production. Beyond its role in sleep regulation, melatonin is a potent mitochondrial antioxidant that protects these organelles from damage. By disrupting natural light-dark cycles, we deprive our mitochondria of this nightly protective treatment, accelerating their decline.
5. Environmental Toxins and Pollution
Heavy metals (like mercury and lead), pesticides, air pollutants, and endocrine-disrupting chemicals from plastics directly damage mitochondrial membranes and interfere with energy production pathways. These toxins can uncouple the electron transport chain—essentially causing mitochondria to leak energy as heat rather than producing ATP efficiently. The constant low-level exposure characteristic of modern environments creates a cumulative burden our ancestors never faced.
6. Nutrient Deficiencies
Mitochondria require specific nutrients as cofactors for energy production. Magnesium activates ATP, iron is essential for electron transport, B vitamins serve as coenzymes in multiple steps, and CoQ10 shuttles electrons within the mitochondrial membrane. Modern farming practices, food processing, and dietary choices often leave us deficient in these mitochondrial essentials, meaning even with sufficient calories, energy production falters.
7. Sedentary Lifestyle and Overtraining Paradox
Both insufficient movement and excessive intense exercise harm mitochondria. Sedentary behavior reduces mitochondrial density and efficiency, while chronic intense training without adequate recovery generates excessive oxidative stress that overwhelms repair mechanisms. The sweet spot—regular, moderate movement—stimulates mitochondrial biogenesis (creation of new mitochondria) without causing destructive overload.
Signs of Mitochondrial Burnout: The Body’s Cellular Distress Signals
Mitochondrial dysfunction rarely appears as a single diagnosable disease in its early stages. Instead, it manifests as a cluster of unexplained symptoms that often puzzle both patients and physicians:
Constant Fatigue Unrelieved by Rest
This isn’t ordinary tiredness but a profound exhaustion that sleep doesn’t resolve—the feeling that your very cells are struggling to generate basic energy for living.
Brain Fog and Memory Issues
Neurons are exceptionally rich in mitochondria because brain activity is energetically expensive. When mitochondrial function declines, cognitive processes suffer first. You might struggle with word retrieval, focus, or short-term memory despite no neurological disease.
Low Motivation and Anhedonia
Dopamine pathways require substantial energy to function properly. Mitochondrial impairment in reward centers of the brain can diminish motivation and pleasure long before mood disorders meet diagnostic criteria.
Muscle Weakness and Poor Exercise Tolerance
Muscle cells contain high concentrations of mitochondria. Early fatigue during activity, prolonged soreness, and weakness despite adequate training may indicate insufficient cellular energy production rather than poor fitness.
Temperature Dysregulation
Cold hands and feet, or general cold intolerance, often reflect poor mitochondrial function since heat production is a byproduct of efficient energy generation.
Mood Changes and Anxiety
The brain’s emotional centers are energy-intensive. Mitochondrial dysfunction in specific brain regions is increasingly linked to anxiety, depression, and emotional volatility.
Slow Recovery from Illness, Stress, or Exercise
When mitochondria can’t produce sufficient energy for immune function and tissue repair, recovery timelines extend noticeably.
Many people presenting with these symptoms are told, “It’s stress” or “just aging,” when the real problem is occurring at the cellular level. This misattribution leads to interventions that address symptoms rather than root causes, often prolonging suffering.
Why Blood Tests Often Look Normal: The Diagnostic Gap
Standard lab tests measure what is circulating in your blood—not what is happening inside your cells. This creates a significant diagnostic blind spot:
You can have normal iron levels in blood, but insufficient iron inside mitochondria where it’s needed for electron transport. Serum iron tests don’t measure cellular or mitochondrial iron status.
Your blood may carry adequate oxygen (normal SpO2), but mitochondria might be unable to utilize it efficiently due to damage to cytochrome c oxidase, the enzyme complex that handles oxygen in the final energy production step.
Thyroid hormones might test within normal range, but cellular conversion of T4 to active T3 occurs within mitochondria—if they’re dysfunctional, you experience hypothyroid symptoms despite normal labs.
Inflammatory markers might be normal in blood while localized cellular inflammation impairs mitochondrial function. Similarly, blood glucose can be normal while cellular insulin resistance starves mitochondria of fuel.
This discrepancy explains why so many people feel unwell despite “perfect” reports. Disease processes begin at the cellular level—sometimes years or decades before they become visible through tissue damage or abnormal blood markers. Mitochondrial dysfunction represents this frontier between optimal health and diagnosable disease.
Who Is Most at Risk? The Modern Mitochondrial Profile
Certain lifestyles and environments create particularly high mitochondrial stress:
Office workers with minimal sunlight exposure face disrupted circadian rhythms and reduced vitamin D, both crucial for mitochondrial function.
Shift workers and those with irregular sleep schedules prevent mitochondria from establishing repair rhythms, leading to accumulated damage.
Individuals under chronic psychological or physiological stress maintain cortisol levels that directly inhibit mitochondrial biogenesis and repair.
Those consuming high sugar, high processed food diets generate constant oxidative stress while lacking necessary nutrients for energy production.
People exposed to urban pollution, mold, or chemical environments face constant toxic burden that damages mitochondrial membranes.
Anyone relying heavily on caffeine and stimulants overrides fatigue signals while depleting nutrients needed for mitochondrial function.
Perfectionists and high achievers often combine several risk factors: chronic stress, sleep sacrifice, reliance on stimulants, and insufficient recovery time.
The common thread is mismatch—between our ancient cellular biology and modern environmental demands. Our mitochondria did not evolve for fluorescent lighting, constant notifications, chronic stress, processed foods, and around-the-clock activity. The result is a growing population experiencing what researchers term “mitochondrial burnout.”
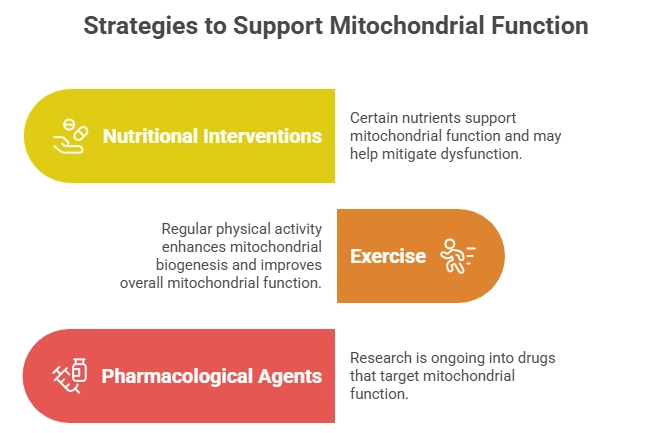
How to Support Your Mitochondria Naturally: Rebuilding Cellular Resilience
You cannot force energy production, but you can create the optimal environment for mitochondria to recover and thrive. The following strategies work synergistically to support mitochondrial health:
1. Prioritize Morning Sunlight Exposure
View sunlight within an hour of waking, even on cloudy days. The specific wavelengths of morning light reset your central circadian clock in the hypothalamus, which in turn synchronizes peripheral clocks in every organ—and within mitochondria themselves. This synchronization improves the efficiency of energy production pathways. Just 10-20 minutes daily can significantly improve mitochondrial function.
2. Stabilize Blood Sugar Through Dietary Rhythm
Rather than merely choosing “healthy foods,” focus on meal timing and composition to avoid glucose spikes. Eat balanced meals containing protein, fiber, and healthy fats at regular intervals. Consider a eating window that aligns with daylight hours (e.g., 10-hour feeding window). This gives mitochondria a predictable fuel supply without oxidative overload and allows nighttime repair periods without digestion competing for energy.
3. Cultivate True Darkness for Sleep
Complete darkness is non-negotiable for mitochondrial repair. Even small amounts of light suppress melatonin, which serves as both sleep hormone and mitochondrial antioxidant. Use blackout curtains, cover electronic lights, and consider an eye mask. Aim for 7-9 hours of quality sleep consistently—the single most effective mitochondrial support strategy.
4. Embrace Gentle, Regular Movement
Walking, cycling, swimming, yoga, and tai chi stimulate mitochondrial biogenesis without generating excessive oxidative stress. The key is consistency rather than intensity. Movement also stimulates autophagy—the cellular cleanup process that removes damaged mitochondria, making way for new, efficient ones.
5. Address Critical Nutrient Deficiencies
Focus on magnesium (critical for ATP structure), B vitamins (especially B1, B2, B3, B5, and B12 as coenzymes in energy production), iron (if deficient), CoQ10 (electron transport), and alpha-lipoic acid (mitochondrial antioxidant). While food sources are ideal, supplementation may be necessary given soil depletion and individual variations in absorption.
6. Strategically Reduce Toxic Load
Progressively minimize exposure by choosing glass or stainless steel over plastic containers, avoiding heating food in plastic, using natural cleaning and personal care products, and installing water and air filters where possible. Even small reductions in toxic burden free mitochondrial resources for energy production rather than detoxification.
7. Practice Strategic Cold Exposure
Brief cold showers or cold water immersion stimulates mitochondrial biogenesis as the body generates heat through non-shivering thermogenesis—a process that occurs in mitochondria-rich brown fat tissue. Start gradually with 30-60 seconds at the end of your shower.
8. Cultivate Circadian Rhythms Beyond Sleep
Consistent meal times, regular movement patterns, and digital sunset (avoiding screens 1-2 hours before bed) reinforce the temporal organization that mitochondria require for optimal function. Chaos at the macro level creates chaos at the cellular level.
9. Incorporate Mitochondrial Nutrients Through Food
Emphasize foods rich in compounds that support mitochondrial function: dark leafy greens (magnesium, folate), nuts and seeds (CoQ10, minerals), fatty fish (omega-3s for membrane fluidity), berries (polyphenols that reduce oxidative stress), and fermented foods (for gut health linked to mitochondrial function).
10. Manage Stress Through Nervous System Regulation
Since chronic stress directly damages mitochondria, daily practices that activate the parasympathetic “rest and digest” system are essential. This might include meditation, deep breathing exercises, nature immersion, or mindful movement. The specific practice matters less than consistent engagement.
Can Mitochondria Recover? The Science of Cellular Renewal
Yes, absolutely. Mitochondria are dynamic organelles that continuously fuse, divide, repair, and are recycled. This process, called mitochondrial dynamics, allows them to adapt to changing energy demands and recover from damage. The body can generate new mitochondria (biogenesis) and remove damaged ones (mitophagy) when given the right signals.
Research shows that mitochondrial improvements can begin within days of positive interventions. Exercise stimulates biogenesis within hours. Dietary changes alter mitochondrial function within days. Sleep restoration initiates repair immediately. Many people notice meaningful changes within weeks:
Improved energy levels not dependent on stimulants
Clearer thinking and better memory recall
Deeper, more restorative sleep
Faster recovery from physical and mental exertion
Improved mood stability and stress resilience
Better temperature regulation
Enhanced exercise performance
The timeline varies based on individual factors including age, genetic predispositions, severity of dysfunction, and consistency of interventions. Younger individuals with shorter exposure to mitochondrial stressors typically recover more quickly, but significant improvement is possible at any age.
Healing begins when you stop forcing the body through stimulants and willpower, and start supporting it through aligned lifestyle choices. This represents a paradigm shift from fighting fatigue to cultivating cellular vitality.
Final Thought: Fatigue as Information, Not Fate
Fatigue is not always a disease—it is often a cellular warning. A signal that the foundational processes sustaining your life are struggling under burdens they did not evolve to handle. In a culture that glorifies pushing through, ignoring signals, and valuing output over vitality, mitochondrial dysfunction represents the physical consequence of living out of alignment with our biology.
Your body is not broken. It is asking for support at the smallest level. The exhaustion you feel might be the most honest feedback you’re receiving—an indication that while you’ve been focused on external achievements, your internal infrastructure requires attention.
When your cells regain power, your life regains momentum. Not the frantic, caffeine-fueled momentum of survival mode, but the steady, sustainable vitality that comes from cellular abundance. This journey back to energy isn’t about adding another supplement or hack to your routine, but about subtracting the burdens that overload your mitochondria and reinforcing the rhythms that allow them to thrive.
In supporting your mitochondria, you’re not just chasing better days or more productivity. You’re engaging in the most fundamental form of self-care: honoring the ancient, delicate, miraculous process that turns sunlight, food, and air into the very experience of being alive. You’re moving from treating symptoms to nurturing the source. And in that shift lies the possibility of not just managing fatigue, but rediscovering what it means to be truly, cellularly vital.
Medical Disclaimer: This article is for educational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider before making health changes.
Dr. Mohammed Abdul Azeem Siddiqui, MBBS, M.Tech (Biomedical Engineering – VIT, Vellore)
Registered Medical Practitioner – Reg. No. 39739
Physician • Clinical Engineer • Preventive Diagnostics Specialist
Dr. Mohammed Abdul Azeem Siddiqui is a physician–engineer with over 30 years of dedicated clinical and biomedical engineering experience, committed to transforming modern healthcare from late-stage disease treatment to early detection, preventive intelligence, and affordable medical care.
He holds an MBBS degree in Medicine and an M.Tech in Biomedical Engineering from VIT University, Vellore, equipping him with rare dual expertise in clinical medicine, laboratory diagnostics, and medical device engineering. This allows him to translate complex laboratory data into precise, actionable preventive strategies.
Clinical Mission
Dr. Siddiqui’s professional mission centers on three core pillars:
Early Disease Detection
Identifying hidden biomarker abnormalities that signal chronic disease years before symptoms appear — reducing complications, hospitalizations, and long-term disability.
Preventive Healthcare
Guiding individuals and families toward longer, healthier lives through structured screenings, lifestyle intervention frameworks, and predictive diagnostic interpretation.
Affordable Evidence-Based Treatment
Delivering cost-effective, scientifically validated care accessible to people from all socioeconomic backgrounds.
Clinical & Technical Expertise
Across three decades of continuous practice, Dr. Siddiqui has worked extensively with:
Advanced laboratory analyzers and automation platforms
• Cardiac, metabolic, renal, hepatic, endocrine, and inflammatory biomarker systems
• Preventive screening and early organ damage detection frameworks
• Clinical escalation pathways and diagnostic decision-support models
• Medical device validation, calibration, compliance, and patient safety standards
He is recognized for identifying subclinical biomarker shifts that predict cardiovascular disease, diabetes, fatty liver, kidney disease, autoimmune inflammation, neurodegeneration, and accelerated biological aging long before conventional diagnosis.
Role at IntelliNewz
At IntelliNewz, Dr. Siddiqui serves as Founder, Chief Medical Editor, and Lead Clinical Validator. Every article published is:
Evidence-based
• Clinically verified
• Technology-grounded
• Free from commercial bias
• Designed for real-world patient and physician decision-making
Through his writing, Dr. Siddiqui shares practical health intelligence, early warning signs, and preventive strategies that readers can trust — grounded in decades of frontline medical practice.
Contact:
powerofprevention@outlook.com
📌 Disclaimer: The content on IntelliNewz is intended for educational purposes only and does not replace personalized medical consultation. For individual health concerns, please consult your physician.