Women’s health is a multifaceted field that includes a wide range of physiological and pathological conditions—many of which uniquely affect women or impact them more severely than men. Genetic factors play a significant role in the development of major diseases such as cancer, cardiovascular disorders, infertility, autoimmune conditions, and pregnancy complications.
Genetic risk assessment—the evaluation of an individual’s likelihood of developing a disease based on their DNA—has become an essential tool in preventive medicine and personalized healthcare.
At the same time, CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats) has emerged as a revolutionary gene-editing technology. It allows scientists to precisely study and potentially correct disease-causing mutations. Together, genetic risk assessment and CRISPR are reshaping how women’s diseases are predicted, prevented, and treated.
Genetic Risk Assessment in Women’s Health
Genetic risk assessment involves analyzing DNA to identify genetic variants associated with an increased risk of disease. It is performed through several methods:
Key Approaches
- Family History Analysis
Evaluates disease patterns across generations to identify inherited risks. - Genetic Testing
Uses blood, saliva, or cheek swabs to detect specific gene mutations such as BRCA1, BRCA2, APOE, and FMR1. - Genome-Wide Association Studies (GWAS)
Examine the entire genome across large populations to identify risk-linked variants.
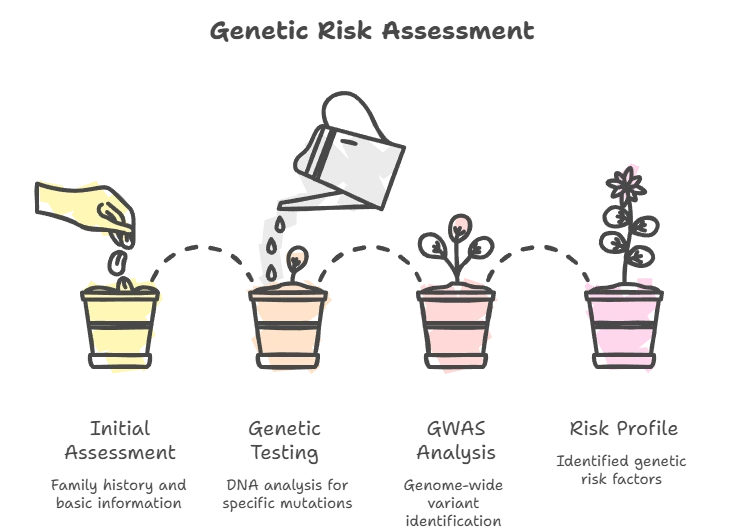
How This Information Is Used
- Personalized Screening & Prevention
Early mammograms, colonoscopies, or hormone screening based on genetic risk. - Informed Reproductive Decisions
Helps assess the risk of passing genetic disorders to children. - Guided Treatment Plans
Allows doctors to choose therapies that match a patient’s genetic profile.
CRISPR Technology: A Brief Overview
CRISPR-Cas9 is a powerful gene-editing system made of two parts:
- Cas9 Enzyme – cuts DNA at a specific location
- Guide RNA (gRNA) – directs Cas9 to the target gene
What CRISPR Can Do
- Knockout Genes – disable harmful genes
- Insert Genes – introduce healthy gene copies
- Repair Genes – correct disease-causing mutations
This makes CRISPR invaluable for understanding disease mechanisms and developing targeted therapies.
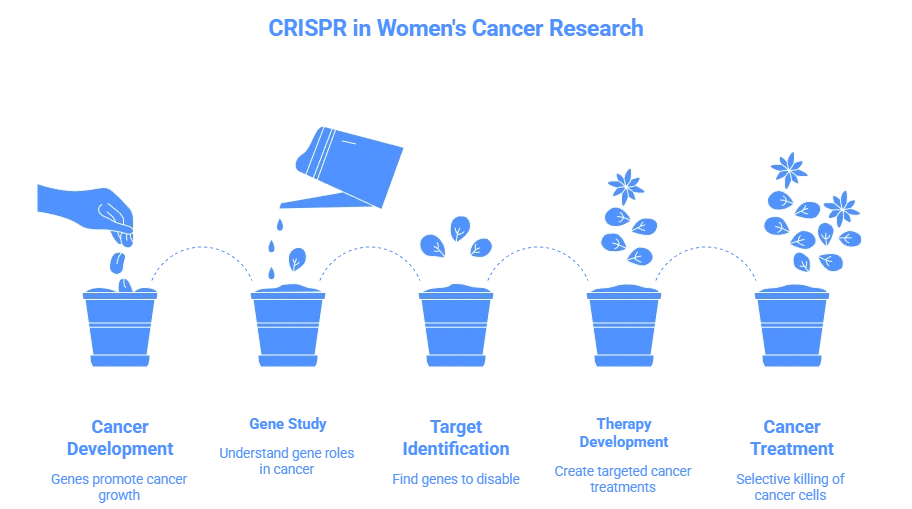
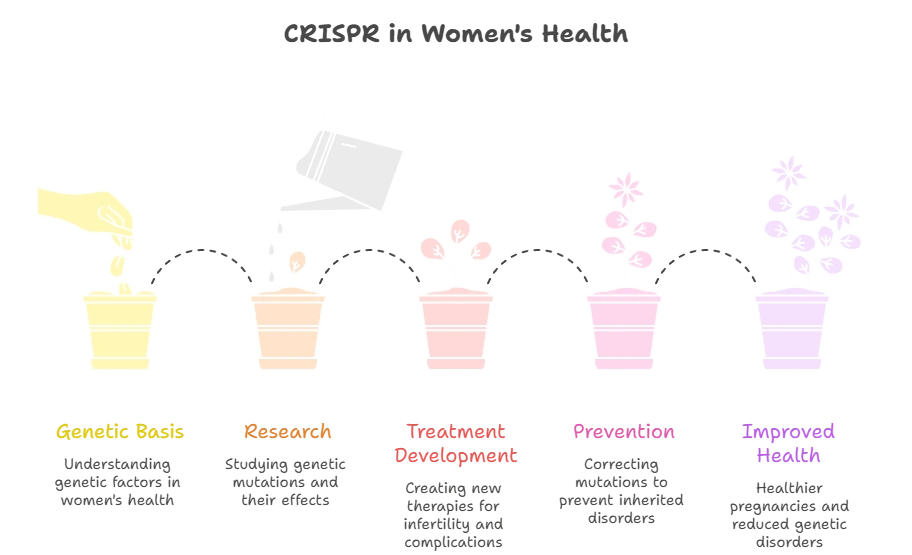
CRISPR Applications in Women’s Health
1. Cancer Research and Therapy
Breast Cancer
CRISPR helps identify genes driving tumor growth and drug resistance, enabling more effective targeted therapies.
Ovarian Cancer
Researchers use CRISPR to disable genes responsible for cancer spread and identify personalized treatment targets.
Cervical Cancer
CRISPR is used to study how HPV interacts with human genes and to develop antiviral gene therapies.
2. Reproductive Health
Infertility
CRISPR is being studied to correct genetic mutations linked to:
- PCOS
- Premature ovarian insufficiency (POI)
- Poor egg development
Pregnancy Complications
CRISPR research helps identify genes involved in:
- Preeclampsia
- Gestational diabetes
- Recurrent miscarriage
Inherited Disorders
While controversial, CRISPR may one day prevent inherited diseases by correcting mutations in embryos.
3. Other Women’s Health Conditions
- Osteoporosis – Gene targets linked to bone density
- Autoimmune Diseases – Lupus and rheumatoid arthritis genes
- Cardiovascular Disease – Post-menopausal risk genes
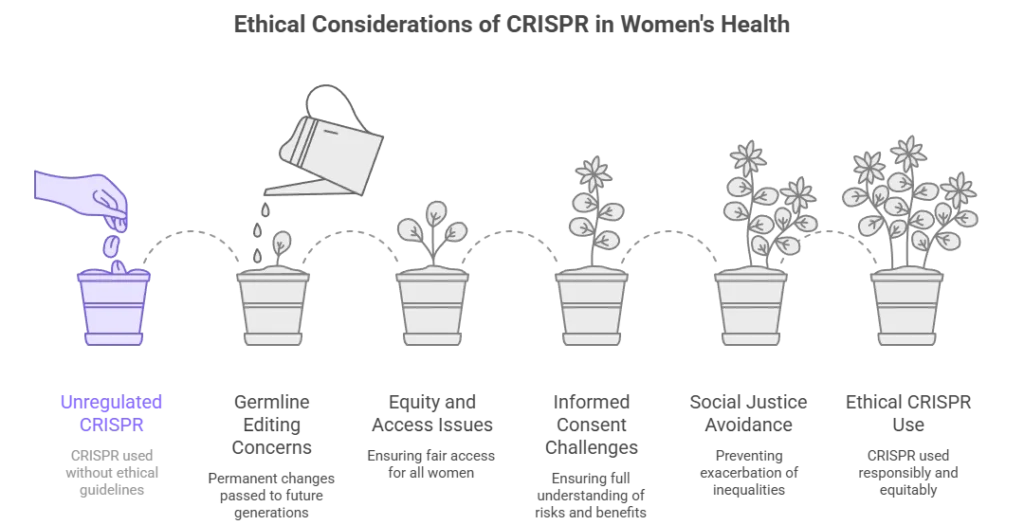
Ethical Considerations
CRISPR raises important ethical questions:
- Germline Editing – Permanent changes passed to future generations
- Equity & Access – Ensuring all women benefit, not only the wealthy
- Informed Consent – Clear understanding of risks and benefits
- Social Justice – Preventing genetic discrimination
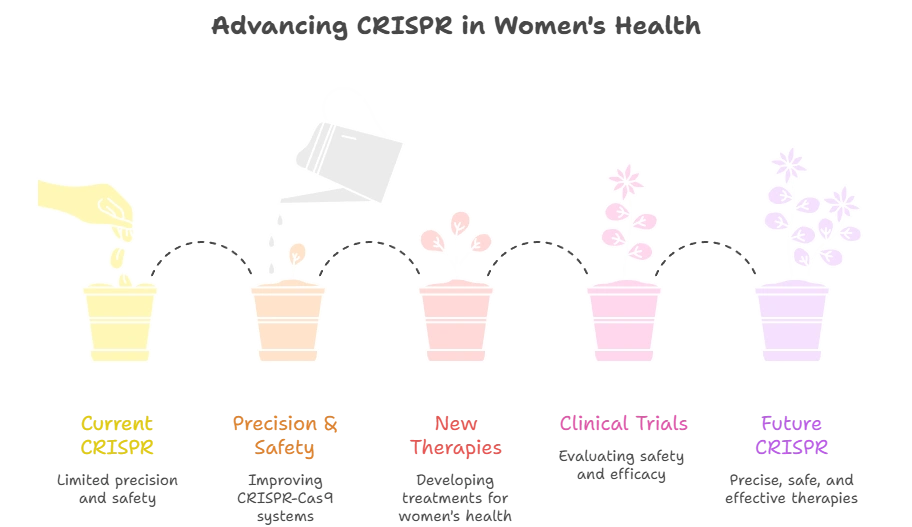
Future Prospects
Researchers are working to:
- Improve CRISPR precision and safety
- Develop FDA-approved gene therapies
- Expand genetic screening
- Integrate AI with DNA analysis
- Establish ethical global standards.
- Clinical Integration: How These Technologies Are Entering Real Healthcare
Although CRISPR is still largely used in research settings, its influence is already shaping clinical decision-making. Genetic risk assessment is now standard practice in many U.S. hospitals, cancer centers, and fertility clinics. As CRISPR research progresses, it is accelerating the discovery of disease-driving genes and helping pharmaceutical companies design gene-targeted therapies.
Hospitals are beginning to integrate genetic dashboards into electronic health records (EHRs), allowing physicians to flag high-risk patients early. For women, this means:
Personalized screening schedules
Risk-based medication selection
Early lifestyle interventions
More accurate fertility planning
This clinical shift marks the beginning of DNA-driven healthcare systems.
The Role of AI and Big Data in Genetic Risk Prediction
Artificial intelligence is now being used to analyze massive genetic databases. Machine learning models can:
Predict disease risk from thousands of gene variants
Identify hidden genetic patterns
Improve polygenic risk scoring accuracy
Forecast treatment responses
When combined with CRISPR lab data, AI allows scientists to test gene functions at unprecedented speed, reducing years of research into months.
This convergence of CRISPR + genetics + AI is creating the foundation of precision medicine.
Environmental and Lifestyle Factors Still Matter
While genetics is powerful, it is not destiny. Studies show that 30–60% of disease risk is influenced by lifestyle and environment.
Women can reduce genetic risk by:
Maintaining healthy weight
Eating anti-inflammatory diets
Managing stress
Avoiding smoking and excess alcohol
Staying physically active
Genetic risk assessment helps identify vulnerability, while lifestyle choices determine expression.
What Women Should Know Before Genetic Testing
Before undergoing genetic testing, women should:
Meet with a genetic counselor
Understand potential emotional impact
Discuss family implications
Review privacy protections
Plan follow-up care
Testing is a tool—not a diagnosis—and must be interpreted in clinical context. - The Long-Term Vision for Women’s Genetic Medicine
In the next decade, experts predict:
Routine genetic screening in primary care
CRISPR-based cancer immunotherapies
Fertility gene correction trials
Preventive care plans based on DNA
Reduced healthcare costs through early intervention
Healthcare is shifting from treatment to prevention at the molecular level. - FAQs:
- Common Questions About CRISPR & Genetic Testing
- Can CRISPR really fix genetic diseases?
- CRISPR can correct disease-causing mutations in laboratory and clinical settings, but most treatments are still in trials and not yet widely available.
- What if I regret genetic testing?
- You can choose not to receive certain results, and many services allow you to withdraw consent or delete your data.
- How private is my DNA data?
- Reputable testing companies use encryption and follow privacy laws, but it’s important to read their data-sharing policies carefully.
- Can genetic testing predict infertility?
- Genetic tests can identify some inherited fertility risks, but they cannot predict all causes of infertility.
- Is CRISPR legal in the U.S.?
- Somatic (non-reproductive) CRISPR gene therapies are legal under FDA regulation. Germline editing is prohibited.
- How much does genetic testing cost?
- Consumer genetic tests usually range from $100 to $300, while medical-grade testing can cost more depending on the panel.
Conclusion
CRISPR and genetic risk assessment are transforming women’s healthcare from reactive to preventive, predictive, and personalized. While challenges remain, responsible use of this technology has the potential to dramatically improve women’s health outcomes worldwide.
Medical Disclaimer
The information provided in this article is for educational and informational purposes only and is not intended as medical advice, diagnosis, or treatment. While every effort has been made to ensure accuracy, the content should not be used as a substitute for professional medical guidance from a qualified healthcare provider.
CRISPR technology and genetic risk assessment are evolving scientific fields. Many applications discussed are currently in research or clinical trial stages and are not yet approved for routine medical use. Individual health conditions, genetic profiles, and treatment responses vary.
Always consult a licensed physician, genetic counselor, or other qualified healthcare professional before making any healthcare decisions, undergoing genetic testing, or changing your treatment plan. Never disregard or delay seeking professional medical advice because of information found in this article.
This website and its authors assume no responsibility for any health outcomes resulting from the use of this information.
Dr. Mohammed Abdul Azeem Siddiqui, MBBS, M.Tech (Biomedical Engineering – VIT, Vellore)
Registered Medical Practitioner – Reg. No. 39739
Physician • Clinical Engineer • Preventive Diagnostics Specialist
Dr. Mohammed Abdul Azeem Siddiqui is a physician–engineer with over 30 years of dedicated clinical and biomedical engineering experience, committed to transforming modern healthcare from late-stage disease treatment to early detection, preventive intelligence, and affordable medical care.
He holds an MBBS degree in Medicine and an M.Tech in Biomedical Engineering from VIT University, Vellore, equipping him with rare dual expertise in clinical medicine, laboratory diagnostics, and medical device engineering. This allows him to translate complex laboratory data into precise, actionable preventive strategies.
Clinical Mission
Dr. Siddiqui’s professional mission centers on three core pillars:
Early Disease Detection
Identifying hidden biomarker abnormalities that signal chronic disease years before symptoms appear — reducing complications, hospitalizations, and long-term disability.
Preventive Healthcare
Guiding individuals and families toward longer, healthier lives through structured screenings, lifestyle intervention frameworks, and predictive diagnostic interpretation.
Affordable Evidence-Based Treatment
Delivering cost-effective, scientifically validated care accessible to people from all socioeconomic backgrounds.
Clinical & Technical Expertise
Across three decades of continuous practice, Dr. Siddiqui has worked extensively with:
Advanced laboratory analyzers and automation platforms
• Cardiac, metabolic, renal, hepatic, endocrine, and inflammatory biomarker systems
• Preventive screening and early organ damage detection frameworks
• Clinical escalation pathways and diagnostic decision-support models
• Medical device validation, calibration, compliance, and patient safety standards
He is recognized for identifying subclinical biomarker shifts that predict cardiovascular disease, diabetes, fatty liver, kidney disease, autoimmune inflammation, neurodegeneration, and accelerated biological aging long before conventional diagnosis.
Role at IntelliNewz
At IntelliNewz, Dr. Siddiqui serves as Founder, Chief Medical Editor, and Lead Clinical Validator. Every article published is:
Evidence-based
• Clinically verified
• Technology-grounded
• Free from commercial bias
• Designed for real-world patient and physician decision-making
Through his writing, Dr. Siddiqui shares practical health intelligence, early warning signs, and preventive strategies that readers can trust — grounded in decades of frontline medical practice.
Contact:
powerofprevention@outlook.com
📌 Disclaimer: The content on IntelliNewz is intended for educational purposes only and does not replace personalized medical consultation. For individual health concerns, please consult your physician.