Fatty liver disease, a condition characterized by the accumulation of excess fat in the liver, is increasingly prevalent worldwide. While often asymptomatic in its early stages, it can progress to more severe liver damage, including cirrhosis and liver failure, if left unaddressed. Fortunately, fatty liver can be reversed, especially when detected early. This document outlines the key blood markers that can indicate the presence of fatty liver disease, enabling timely intervention and lifestyle modifications to halt its progression and potentially reverse its effects.

Fatty Liver Is Now One of the Fastest-Growing Silent Diseases
Non-alcoholic fatty liver disease (NAFLD) is rapidly becoming one of the leading causes of cirrhosis and liver cancer worldwide.
The most dangerous aspect is that fatty liver develops silently. Most people feel completely healthy while their liver accumulates fat, inflammation, and microscopic scarring.
Routine liver enzymes often remain normal until irreversible damage has already occurred.
Today, modern biomarkers allow early detection and reversal.
Why Routine Liver Tests Miss Fatty Liver
Standard liver tests only detect late-stage damage:
• ALT
• AST
• ALP
• Bilirubin
These rise only after significant fibrosis or cirrhosis develops.
Fatty liver actually begins with:
• Insulin resistance
• Mitochondrial dysfunction
• Oxidative stress
• Fibrotic scarring
These are invisible on routine labs.
The Liver Marker That Changed Prevention: ELF Score
The ELF (Enhanced Liver Fibrosis) Score detects microscopic liver scarring years before cirrhosis develops.
It measures three fibrosis markers:
• Hyaluronic acid
• PIIINP
• TIMP-1
High ELF predicts progression to cirrhosis, liver failure, and liver cancer — often 10–15 years before symptoms appear.
Additional Early Liver Damage Markers
| Biomarker | What It Detects |
|---|---|
| FGF-21 | Metabolic liver stress |
| miR-122 | Hepatocyte injury |
| Cytokeratin-18 | Liver cell apoptosis |
| TyG Index | Insulin resistance |
| Ferritin | Iron-induced liver injury |
Who Should Get Early Screening?
• Adults over 30
• People with abdominal obesity
• Diabetics or pre-diabetics
• Individuals with fatigue, bloating, or poor digestion
• Anyone with family history of liver disease
This prevents cirrhosis, transplant, and liver cancer.
Fatty Liver Is Reversible — If Found Early
Early-stage fatty liver can be completely reversed with:
• Weight normalization
• Insulin sensitivity correction
• Anti-inflammatory nutrition
• Alcohol moderation
• Sleep and stress optimization
Fatty liver does not announce itself — but biomarkers do.
Early detection gives your liver a second chance.
Understanding Fatty Liver Disease
Fatty liver disease encompasses a spectrum of conditions, ranging from simple steatosis (fat accumulation) to nonalcoholic steatohepatitis (NASH), which involves inflammation and liver cell damage. The primary causes include obesity, insulin resistance, high cholesterol, and poor dietary habits. Early detection is crucial because lifestyle changes and medical interventions are most effective in the initial stages of the disease.
Key Blood Markers for Early Detection
Several blood markers can provide valuable insights into liver health and help identify fatty liver disease in its early stages:
1. Liver Enzymes: ALT and AST
Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are liver enzymes that are released into the bloodstream when liver cells are damaged. Elevated levels of ALT and AST are common indicators of liver inflammation and injury, often associated with fatty liver disease.
- ALT (Alanine Aminotransferase): ALT is more specific to the liver than AST. Elevated ALT levels are a strong indicator of liver damage. Normal range is typically between 7 to 55 U/L, but this can vary slightly between labs.
- AST (Aspartate Aminotransferase): While AST is also found in other organs, elevated levels along with ALT can suggest liver issues. Normal range is typically between 8 to 48 U/L, but this can vary slightly between labs.
It’s important to note that elevated ALT and AST levels can also be caused by other conditions, such as alcohol abuse, certain medications, and viral hepatitis. Therefore, further investigation is necessary to confirm the diagnosis of fatty liver disease.
2. Gamma-Glutamyl Transferase (GGT)
Gamma-glutamyl transferase (GGT) is another liver enzyme that can be elevated in individuals with fatty liver disease. GGT is involved in the metabolism of drugs and toxins, and its levels can increase in response to liver damage or inflammation.
- GGT (Gamma-Glutamyl Transferase): Elevated GGT levels can indicate liver damage, bile duct obstruction, or alcohol abuse. Normal range is typically between 9 to 48 U/L, but this can vary slightly between labs.
While GGT is not as specific to the liver as ALT, it can provide additional information about liver health, especially when considered in conjunction with other liver enzymes.
3. Alkaline Phosphatase (ALP)
Alkaline phosphatase (ALP) is an enzyme found in the liver, bones, and other tissues. Elevated ALP levels can indicate liver damage, bile duct obstruction, or bone disorders.
- ALP (Alkaline Phosphatase): Elevated ALP levels can indicate liver damage, bile duct obstruction, or bone disorders. Normal range is typically between 44 to 147 U/L, but this can vary slightly between labs.
In the context of fatty liver disease, elevated ALP levels may suggest that the condition has progressed to involve bile duct inflammation or obstruction.
4. Bilirubin
Bilirubin is a yellow pigment produced during the breakdown of red blood cells. The liver processes bilirubin and excretes it in bile. Elevated bilirubin levels can indicate liver damage or bile duct obstruction.
- Bilirubin: Elevated bilirubin levels can indicate liver damage or bile duct obstruction. Normal range for total bilirubin is typically between 0.3 to 1.0 mg/dL, but this can vary slightly between labs.
In fatty liver disease, elevated bilirubin levels may suggest that the liver is struggling to process bilirubin effectively, indicating more severe liver dysfunction.
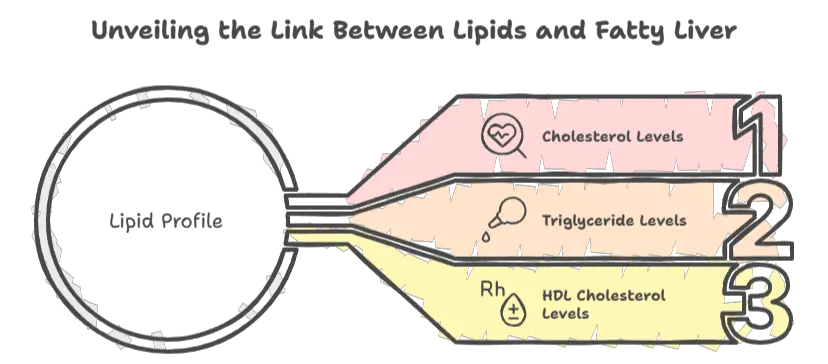
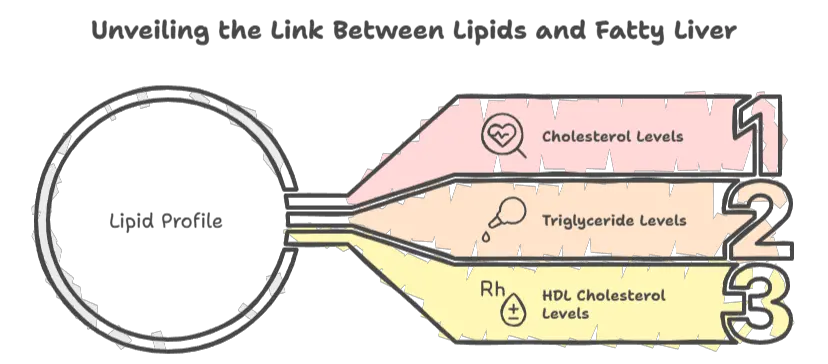
5. Lipid Profile
A lipid profile measures the levels of cholesterol and triglycerides in the blood. Abnormal lipid levels, such as high triglycerides and low HDL cholesterol, are commonly associated with fatty liver disease.
- Triglycerides: High triglyceride levels are often seen in individuals with fatty liver disease.
- HDL Cholesterol: Low HDL cholesterol levels are also associated with fatty liver disease.
Monitoring lipid levels can help assess the risk of fatty liver disease and guide treatment strategies, such as dietary modifications and medications to lower cholesterol and triglycerides.
6. Fasting Blood Sugar and HbA1c
Fasting blood sugar and HbA1c (glycated hemoglobin) are measures of blood sugar control. Insulin resistance and type 2 diabetes are major risk factors for fatty liver disease.
- Fasting Blood Sugar: Elevated fasting blood sugar levels can indicate insulin resistance or diabetes.
- HbA1c: HbA1c provides an average measure of blood sugar levels over the past 2-3 months. Elevated HbA1c levels indicate poor blood sugar control.
Monitoring fasting blood sugar and HbA1c can help identify individuals at risk of fatty liver disease and guide interventions to improve blood sugar control, such as lifestyle changes and medications.
7. Ferritin
Ferritin is a protein that stores iron in the body. Elevated ferritin levels can indicate iron overload, which can contribute to liver damage and inflammation.
- Ferritin: Elevated ferritin levels can indicate iron overload, which can contribute to liver damage and inflammation.
In the context of fatty liver disease, elevated ferritin levels may suggest that iron overload is contributing to liver damage.
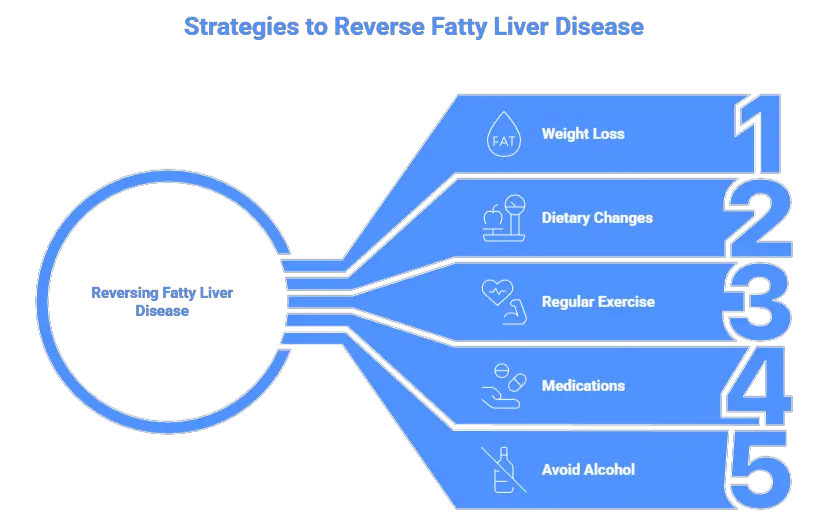
Reversing Fatty Liver Disease
If these blood markers are found early, fatty liver disease can often be reversed through lifestyle modifications and medical interventions:
- Weight Loss: Losing even a modest amount of weight (5-10% of body weight) can significantly reduce liver fat and inflammation.
- Dietary Changes: Adopting a healthy diet that is low in saturated fats, refined carbohydrates, and added sugars can improve liver health.
- Regular Exercise: Engaging in regular physical activity can help reduce liver fat and improve insulin sensitivity.
- Medications: In some cases, medications may be necessary to treat underlying conditions, such as diabetes or high cholesterol, that contribute to fatty liver disease.
- Avoid Alcohol: Abstaining from alcohol is crucial, as alcohol can exacerbate liver damage.
Conclusion
Early detection of fatty liver disease is essential for preventing its progression to more severe liver damage. Monitoring key blood markers, such as liver enzymes, lipid profile, fasting blood sugar, and ferritin, can help identify individuals at risk and guide timely interventions. By adopting healthy lifestyle changes and seeking appropriate medical care, it is often possible to reverse fatty liver disease and improve overall liver health. Regular check-ups and awareness of these blood markers are vital for maintaining liver health and preventing the long-term complications of fatty liver disease.
Medical Disclaimer
Educational only. Consult your healthcare provider before testing.
Dr. Mohammed Abdul Azeem Siddiqui, MBBS, M.Tech (Biomedical Engineering – VIT, Vellore)
Registered Medical Practitioner – Reg. No. 39739
Physician • Clinical Engineer • Preventive Diagnostics Specialist
Dr. Mohammed Abdul Azeem Siddiqui is a physician–engineer with over 30 years of dedicated clinical and biomedical engineering experience, committed to transforming modern healthcare from late-stage disease treatment to early detection, preventive intelligence, and affordable medical care.
He holds an MBBS degree in Medicine and an M.Tech in Biomedical Engineering from VIT University, Vellore, equipping him with rare dual expertise in clinical medicine, laboratory diagnostics, and medical device engineering. This allows him to translate complex laboratory data into precise, actionable preventive strategies.
Clinical Mission
Dr. Siddiqui’s professional mission centers on three core pillars:
Early Disease Detection
Identifying hidden biomarker abnormalities that signal chronic disease years before symptoms appear — reducing complications, hospitalizations, and long-term disability.
Preventive Healthcare
Guiding individuals and families toward longer, healthier lives through structured screenings, lifestyle intervention frameworks, and predictive diagnostic interpretation.
Affordable Evidence-Based Treatment
Delivering cost-effective, scientifically validated care accessible to people from all socioeconomic backgrounds.
Clinical & Technical Expertise
Across three decades of continuous practice, Dr. Siddiqui has worked extensively with:
Advanced laboratory analyzers and automation platforms
• Cardiac, metabolic, renal, hepatic, endocrine, and inflammatory biomarker systems
• Preventive screening and early organ damage detection frameworks
• Clinical escalation pathways and diagnostic decision-support models
• Medical device validation, calibration, compliance, and patient safety standards
He is recognized for identifying subclinical biomarker shifts that predict cardiovascular disease, diabetes, fatty liver, kidney disease, autoimmune inflammation, neurodegeneration, and accelerated biological aging long before conventional diagnosis.
Role at IntelliNewz
At IntelliNewz, Dr. Siddiqui serves as Founder, Chief Medical Editor, and Lead Clinical Validator. Every article published is:
Evidence-based
• Clinically verified
• Technology-grounded
• Free from commercial bias
• Designed for real-world patient and physician decision-making
Through his writing, Dr. Siddiqui shares practical health intelligence, early warning signs, and preventive strategies that readers can trust — grounded in decades of frontline medical practice.
Contact:
powerofprevention@outlook.com
📌 Disclaimer: The content on IntelliNewz is intended for educational purposes only and does not replace personalized medical consultation. For individual health concerns, please consult your physician.