Why this matters
Breast cancer is most treatable when it is caught early. Yet every year in the United States, tens of thousands of women are diagnosed only after the disease has already grown into a tumor large enough to appear on a mammogram.
Modern science is now using a gene-editing tool called CRISPR to find cancer at the genetic level, sometimes years before imaging can.
This shift could change how cancer is detected, treated, and survived.
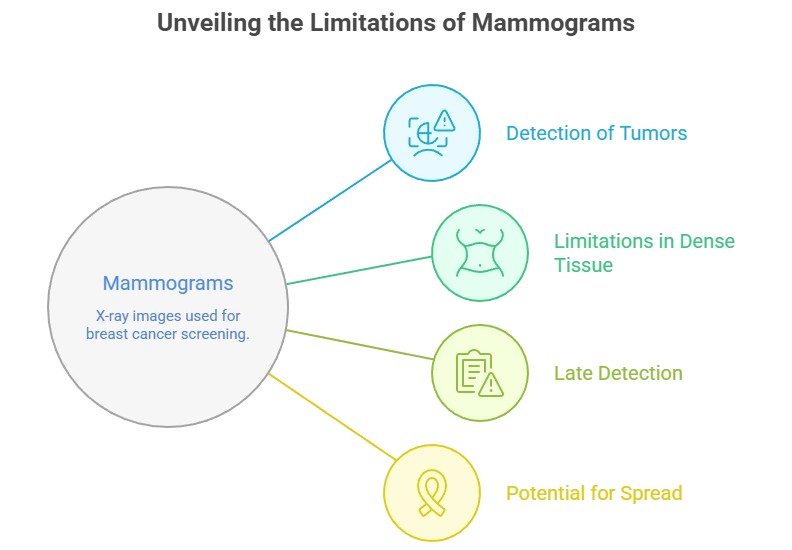
Why mammograms miss early cancer
Mammograms are X-ray images. They work by looking for physical changes in breast tissue such as:
- Lumps
- Calcifications
- Tissue distortion
But cancer does not begin as a lump.
Cancer begins when DNA inside a cell mutates, causing the cell to divide uncontrollably. At first:
- There is no mass
- No visible shape
- No structural change
It may take years before those abnormal cells grow into something large enough to be seen on imaging.
This creates a dangerous blind spot
By the time a tumor is visible on a mammogram:
- Millions or billions of cancer cells already exist
- Some may have started spreading
- The cancer may be harder to treat
This is why some aggressive breast cancers appear “between screenings.”
What CRISPR actually does
CRISPR is best known as a gene-editing tool, but in medicine it is also being used as a genetic sensor.
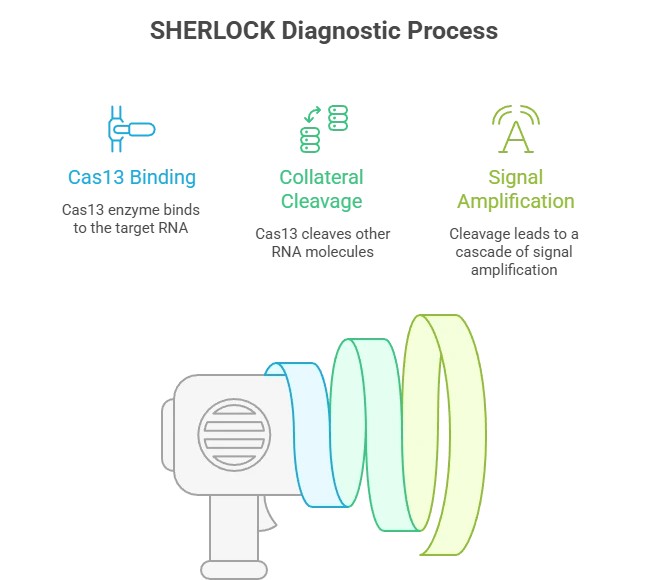
Scientists have adapted CRISPR to:
- Detect cancer DNA
- Find tumor-specific mutations
- Identify microscopic cancer fragments in blood
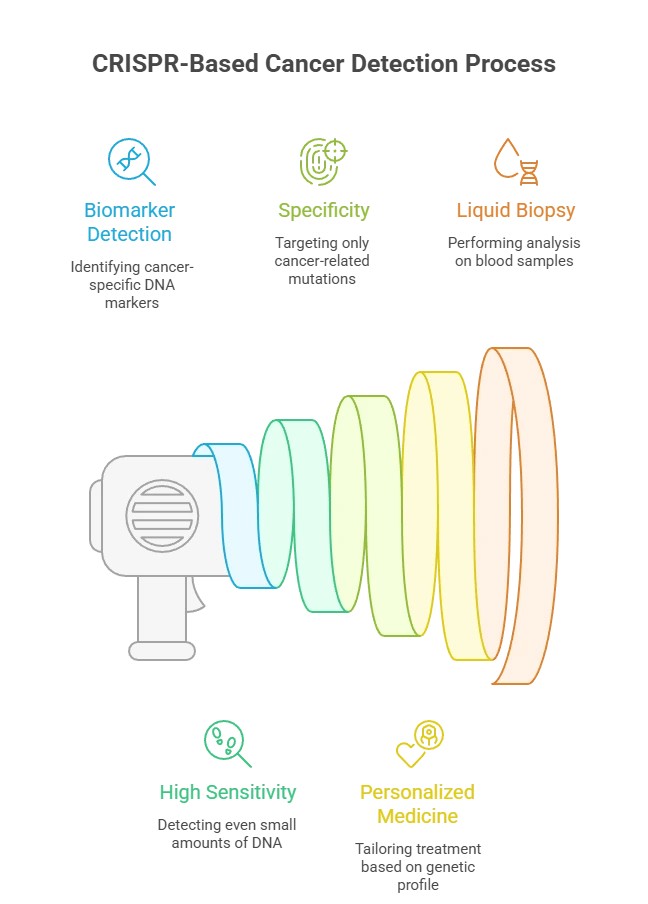
These tests are called CRISPR-based liquid biopsies.
Instead of looking for a tumor, they look for cancer’s genetic fingerprint.
How CRISPR detects cancer before scans can
Cancer cells shed tiny pieces of DNA into the bloodstream. These fragments are called circulating tumor DNA (ctDNA).
CRISPR can be programmed to:
- Search for specific cancer mutations
- Bind only to tumor DNA
- Light up or signal when cancer DNA is present
This means a simple blood draw could detect:
- Breast cancer
- Ovarian cancer
- Endometrial cancer
- Even very early disease
Before any lump forms.
Why this is revolutionary for women’s health
Women’s cancers often go undetected because:
- Ovarian cancer rarely causes early symptoms
- Endometrial cancer can hide until it spreads
- Dense breast tissue makes mammograms less reliable
CRISPR tests can bypass all of this because:
- They don’t rely on imaging
- They don’t need symptoms
- They don’t need a tumor to exist
They detect the disease at its molecular origin.
What this means for early detection
Traditional screening asks:
“Is there a tumor yet?”
CRISPR asks:
“Has cancer started?”
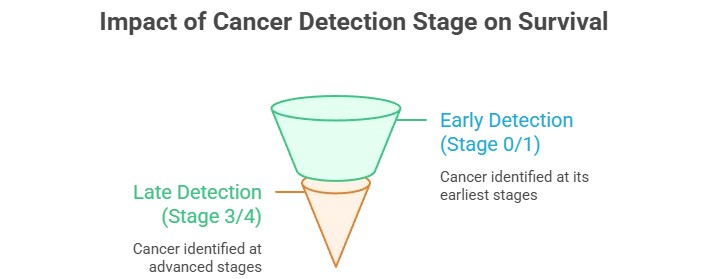
That difference can mean:
- Earlier diagnosis
- Less aggressive treatment
- Higher survival rates
- Lower healthcare costs
For breast cancer alone, early detection raises survival above 90%.
Are CRISPR cancer tests available now?
Some CRISPR-based cancer blood tests are already in:
- Clinical trials
- Research hospitals
- Specialized cancer centers
They are not yet part of routine screening, but they are moving fast.
Many experts believe they will be used alongside mammograms and ultrasounds within the next decade.
Will CRISPR replace mammograms?
No — but it will change how they are used.
Future screening will likely look like this:
- Blood test finds cancer DNA
- Imaging locates the tumor
- Treatment starts earlier
CRISPR becomes the early warning system.
Mammograms become the mapping tool.
What women should know today
If you are a woman in the U.S., especially if you:
- Have a family history of cancer
- Have dense breasts
- Have unexplained symptoms
You should know:
Normal imaging does not always mean no cancer.
Genetic testing is becoming the next frontier of prevention.
The future of cancer screening
Cancer does not start as a lump.
It starts as a genetic error.
CRISPR is the first technology powerful enough to see that error while it is still invisible.
This could be one of the most important advances in women’s health in our lifetime.
Answers from experts on the questions most people don’t know about mammograms, CRISPR, and early cancer detection.
How Cancer Really Begins
Does cancer start as a lump?
No. Cancer usually begins with DNA mutations long before a lump forms.
What is a genetic mutation?
A mutation is a change in DNA that can disrupt normal cell behavior.
Can cancer begin in a single cell?
Yes. One damaged cell can start uncontrolled growth.
How long can cancer exist without symptoms?
Some cancers grow silently for many years.
Is cancer always inherited?
No. Most cancers result from mutations acquired during life.
Why doesn’t the body stop mutated cells?
Cancer cells can bypass normal growth controls.
What is the earliest stage of cancer?
The molecular stage, when DNA damage first occurs.
Do all mutations cause cancer?
No. Many mutations are harmless.
Can DNA repair itself?
Often yes, but repair mechanisms sometimes fail.
Can cancer start years before detection?
Yes. Many cancers begin long before diagnosis.
Why Mammograms and Scans Have Limits
What does a mammogram detect?
It detects physical changes in breast tissue.
Why can mammograms miss early cancer?
They cannot detect DNA-level changes.
Can imaging tests see genetic mutations?
No. Imaging only shows structure, not molecules.
Does dense breast tissue affect results?
Yes. Dense tissue can hide tumors.
Are mammograms still important?
Yes. They are vital for detecting existing tumors.
Can scans predict cancer risk?
No. Risk comes from genetics and biology.
Are false negatives possible?
Yes. No test is perfect.
Why must a tumor form before detection?
Imaging requires visible tissue changes.
Are MRIs better than mammograms?
MRIs can help in high-risk cases but still don’t see DNA.
Do scans detect all cancers?
No. Some cancers remain invisible early on.
Genetics, DNA, and Cancer Risk
What genes are linked to cancer?
Genes like BRCA1 and BRCA2 are well known.
Can lifestyle cause DNA damage?
Yes. Smoking, diet, and toxins can affect DNA.
Does aging increase mutation risk?
Yes. Mutations accumulate over time.
Can stress damage DNA?
Chronic stress may indirectly affect cellular health.
Is genetic testing useful?
It helps assess cancer risk, not diagnose cancer.
Who should consider genetic testing?
Those with strong family history.
Can diet protect DNA?
Healthy diets support cellular repair.
Are genetic mutations common?
Yes. Everyone has mutations.
Can family history predict cancer?
It increases risk but does not guarantee cancer.
Is genetic damage reversible?
Some damage can be repaired by cells.
CRISPR and Genetic Technologies
What is CRISPR?
A tool that allows precise interaction with DNA.
How does CRISPR work?
It targets specific genetic sequences.
Can CRISPR detect cancer?
In research, it helps identify cancer mutations.
Is CRISPR used in humans?
It is used in controlled clinical research.
Is CRISPR FDA approved?
Some CRISPR therapies are in clinical trials.
Can CRISPR replace mammograms?
No. It complements imaging.
How precise is CRISPR?
Extremely precise at the DNA level.
Is CRISPR safe?
Safety is carefully studied in trials.
What are CRISPR limitations?
Delivery and long-term effects are challenges.
Is CRISPR used in diagnostics?
Yes, in experimental diagnostic tools.
Early Detection and Liquid Biopsies
What is early cancer detection?
Finding cancer before symptoms appear.
Can blood tests detect cancer?
Some tests detect cancer DNA fragments.
What is a liquid biopsy?
A blood test that looks for tumor DNA.
How accurate are liquid biopsies?
Accuracy varies by cancer type.
Are liquid biopsies widely available?
Some are available; many are still in trials.
Can cancer be detected before symptoms?
Yes, in some cases.
Can early detection save lives?
Earlier detection improves survival.
Are early tests expensive?
Costs are decreasing.
Who qualifies for early screening?
High-risk individuals may qualify.
When will early detection be common?
Experts expect wider use in coming years.
Prevention, Treatment, and the Future
Can cancer be prevented genetically?
Research is exploring early intervention.
Is early genetic detection ethical?
Ethics are carefully considered.
Will cancer screening change?
Yes. Genetic tools will play a bigger role.
Is cancer always fatal?
No. Many cancers are treatable.
What is precision medicine?
Treatment tailored to genetic profiles.
Will genetic screening be routine?
Likely in the future.
Can early treatment stop tumors?
Early treatment improves outcomes.
Will scans become obsolete?
No. Imaging remains essential.
What should patients do now?
Follow screening guidelines and consult doctors.
What is the future of cancer detection?
Earlier, more precise, and personalized.
What type of breast cancer does not show up on a mammogram?
Several types of breast cancer can be difficult or impossible to see on a mammogram, especially in early stages:
- Inflammatory breast cancer (IBC)
This aggressive cancer often does not form a distinct lump. Instead, it causes skin redness, swelling, or warmth, which may not appear as a clear mass on imaging. - Invasive lobular carcinoma (ILC)
ILC spreads in a sheet-like pattern, not as a round tumor, making it harder to detect on mammograms. - Breast cancer in dense breast tissue
Dense tissue appears white on a mammogram—the same color as tumors—so cancers can be masked.
What is the best early detection strategy for breast cancer?
There is no single perfect test. The most effective early detection strategy combines multiple approaches:
- Regular mammograms (starting at age 40–50, based on risk)
- Clinical breast exams
- Breast MRI or ultrasound for high-risk women or dense breasts
- Genetic testing for women with family history or known mutations (BRCA1/2)
- Emerging blood-based tests (liquid biopsy) that look for cancer DNA
Early detection works best when genetic, imaging, and clinical tools are used together, not in isolation.
What type of cancer is easily missed on a mammogram?
Cancers most often missed include:
- Early-stage breast cancer (before a tumor forms)
- Fast-growing aggressive cancers that appear between screenings
- Cancers in younger women with dense breast tissue
- Lobular and inflammatory breast cancers
Mammograms detect physical changes, not the genetic changes that start cancer.
What is the new test instead of a mammogram?
There is no full replacement yet, but a promising new approach is:
CRISPR-based blood tests (liquid biopsies)
These tests:
- Detect circulating tumor DNA (ctDNA) in blood
- Identify cancer before a lump forms
- Work even when imaging looks normal
- Are being studied for breast, ovarian, and other cancers
⚠️ Important:
CRISPR blood tests are not a replacement for mammograms today, but they may soon be used alongside imaging as an early-warning system.
Key takeaway for the public
- Mammograms save lives—but they do not catch all cancers
- Cancer starts in DNA, not as a lump
- New genetic blood tests may help detect cancer earlier than imaging
- The future of breast cancer screening is combined testing, not one test alone
FAQs:
What type of breast cancer does not show up on a mammogram?
Several types of breast cancer can be difficult or impossible to see on a mammogram, especially in early stages:
- Inflammatory breast cancer (IBC)
This aggressive cancer often does not form a distinct lump. Instead, it causes skin redness, swelling, or warmth, which may not appear as a clear mass on imaging. - Invasive lobular carcinoma (ILC)
ILC spreads in a sheet-like pattern, not as a round tumor, making it harder to detect on mammograms. - Breast cancer in dense breast tissue
Dense tissue appears white on a mammogram—the same color as tumors—so cancers can be masked.
What is the best early detection strategy for breast cancer?
There is no single perfect test. The most effective early detection strategy combines multiple approaches:
- Regular mammograms (starting at age 40–50, based on risk)
- Clinical breast exams
- Breast MRI or ultrasound for high-risk women or dense breasts
- Genetic testing for women with family history or known mutations (BRCA1/2)
- Emerging blood-based tests (liquid biopsy) that look for cancer DNA
Early detection works best when genetic, imaging, and clinical tools are used together, not in isolation.
What type of cancer is easily missed on a mammogram?
Cancers most often missed include:
- Early-stage breast cancer (before a tumor forms)
- Fast-growing aggressive cancers that appear between screenings
- Cancers in younger women with dense breast tissue
- Lobular and inflammatory breast cancers
Mammograms detect physical changes, not the genetic changes that start cancer.
What is the new test instead of a mammogram?
There is no full replacement yet, but a promising new approach is:
CRISPR-based blood tests (liquid biopsies)
These tests:
- Detect circulating tumor DNA (ctDNA) in blood
- Identify cancer before a lump forms
- Work even when imaging looks normal
- Are being studied for breast, ovarian, and other cancers
⚠️ Important:
CRISPR blood tests are not a replacement for mammograms today, but they may soon be used alongside imaging as an early-warning system.
Primary Medical Sources
- American Cancer Society (ACS)
Limitations of Mammograms & Dense Breast Tissue
https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection.html - National Cancer Institute (NCI)
Liquid Biopsies and Circulating Tumor DNA
https://www.cancer.gov/about-cancer/diagnosis-staging/liquid-biopsy - U.S. Food & Drug Administration (FDA)
Mammography & Breast Cancer Screening
https://www.fda.gov/radiation-emitting-products/mqsa-insights/mammography - Johns Hopkins Medicine
Inflammatory and Lobular Breast Cancer Detection Challenges
https://www.hopkinsmedicine.org/health/conditions-and-diseases/breast-cancer - Nature Biotechnology / Science Translational Medicine
CRISPR-Based Diagnostics for Cancer Detection
(Widely cited peer-reviewed research on CRISPR diagnostics and liquid biopsy applications)
Medical Disclaimer
The content on this page is for educational and informational purposes only and is not intended as medical advice. It does not replace consultation with a qualified healthcare professional.
- Always consult your doctor, nurse, or other qualified healthcare provider regarding screening, diagnosis, or treatment options for breast cancer or any other medical condition.
- The information about mammograms, CRISPR tests, and other cancer detection methods is general and may not apply to your individual situation.
- CRISPR-based blood tests are emerging technologies and are not yet a replacement for standard medical screening.
- Reliance on any information provided on this website is solely at your own risk.
For personalized advice, please speak with a licensed healthcare professional.
Contact: powerofprevention@outlook.com
Dr. Mohammed Abdul Azeem Siddiqui, MBBS, M.Tech (Biomedical Engineering – VIT, Vellore)
Registered Medical Practitioner – Reg. No. 39739
Physician • Clinical Engineer • Preventive Diagnostics Specialist
Dr. Mohammed Abdul Azeem Siddiqui is a physician–engineer with over 30 years of dedicated clinical and biomedical engineering experience, committed to transforming modern healthcare from late-stage disease treatment to early detection, preventive intelligence, and affordable medical care.
He holds an MBBS degree in Medicine and an M.Tech in Biomedical Engineering from VIT University, Vellore, equipping him with rare dual expertise in clinical medicine, laboratory diagnostics, and medical device engineering. This allows him to translate complex laboratory data into precise, actionable preventive strategies.
Clinical Mission
Dr. Siddiqui’s professional mission centers on three core pillars:
Early Disease Detection
Identifying hidden biomarker abnormalities that signal chronic disease years before symptoms appear — reducing complications, hospitalizations, and long-term disability.
Preventive Healthcare
Guiding individuals and families toward longer, healthier lives through structured screenings, lifestyle intervention frameworks, and predictive diagnostic interpretation.
Affordable Evidence-Based Treatment
Delivering cost-effective, scientifically validated care accessible to people from all socioeconomic backgrounds.
Clinical & Technical Expertise
Across three decades of continuous practice, Dr. Siddiqui has worked extensively with:
Advanced laboratory analyzers and automation platforms
• Cardiac, metabolic, renal, hepatic, endocrine, and inflammatory biomarker systems
• Preventive screening and early organ damage detection frameworks
• Clinical escalation pathways and diagnostic decision-support models
• Medical device validation, calibration, compliance, and patient safety standards
He is recognized for identifying subclinical biomarker shifts that predict cardiovascular disease, diabetes, fatty liver, kidney disease, autoimmune inflammation, neurodegeneration, and accelerated biological aging long before conventional diagnosis.
Role at IntelliNewz
At IntelliNewz, Dr. Siddiqui serves as Founder, Chief Medical Editor, and Lead Clinical Validator. Every article published is:
Evidence-based
• Clinically verified
• Technology-grounded
• Free from commercial bias
• Designed for real-world patient and physician decision-making
Through his writing, Dr. Siddiqui shares practical health intelligence, early warning signs, and preventive strategies that readers can trust — grounded in decades of frontline medical practice.
Contact:
powerofprevention@outlook.com
📌 Disclaimer: The content on IntelliNewz is intended for educational purposes only and does not replace personalized medical consultation. For individual health concerns, please consult your physician.