Introduction: The Mystery of the “Normal” Blood Test
You feel exhausted all the time. Your brain feels foggy, your hair is thinning, and you’re battling persistent muscle aches. Yet, when you finally see your doctor and get a full panel of blood tests, the results come back stamped: “Within Normal Limits.” You’re told everything is fine, but you know your body is telling a different story. This frustrating scenario is more common than you might think, and it often points to a critical, overlooked flaw in conventional medical testing: The False Deficiency Trap.
# The False Deficiency Trap: Your Questions Answered Below are answers to the most common questions about why standard blood tests can miss critical cellular nutrient deficiencies. Click on any question to reveal the detailed answer. ## General Understanding & BasicsWhat exactly is the “False Deficiency” trap?
The “False Deficiency” trap occurs when standard blood tests show nutrient levels within the “normal” reference range, while your actual cells—where the biochemical work happens—are deficient. This happens because serum tests (the liquid part of your blood) measure what’s in transit to your cells, not what has actually been absorbed and utilized inside them. Think of it as checking delivery trucks on a highway (serum) versus checking inventory inside the factory (cells). The factory can be nearly empty while the highway looks busy.
How can a blood test be normal but I still feel sick?
Because standard blood tests have significant limitations. They measure extracellular fluid, not intracellular status. Your body is biologically programmed to keep serum levels of critical nutrients (like magnesium, potassium) stable at all costs—it will strip these minerals from your bones and muscles to maintain a normal blood reading. So, you can have debilitating symptoms of cellular starvation (fatigue, muscle cramps, brain fog) while your serum labs appear perfectly fine. Your symptoms are real data pointing to a problem the standard test isn’t designed to detect.
Why haven’t I heard about this from my doctor?
Mainstream medical training and standard-of-care protocols are built around diagnosing pathology—overt disease states. The “False Deficiency” trap exists in the subtler realm of functional medicine, which focuses on optimal cellular function and prevention. Most doctors rely on serum tests because they’re standardized, widely available, and insurance-covered. The concept of cellular-level deficiencies, while backed by growing research, is not yet part of conventional medical education for most primary care physicians.
Why does the body prioritize serum levels over cellular levels?
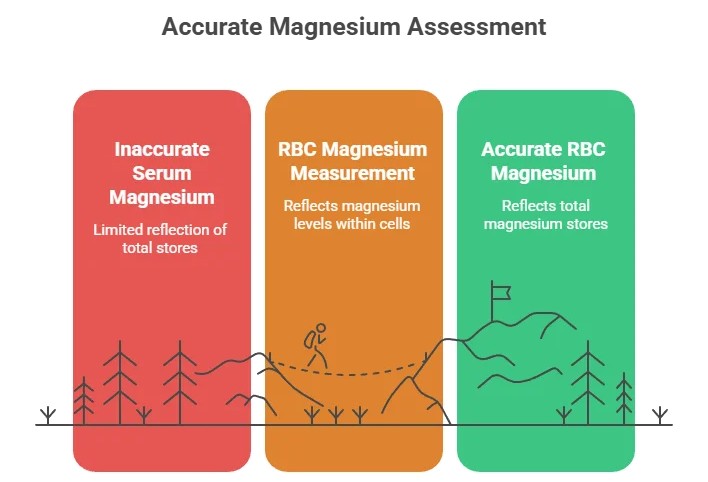
It’s a survival mechanism called homeostasis. Your body maintains stable serum levels of electrolytes like magnesium and potassium because sudden drops in blood concentration can cause immediate, life-threatening problems like cardiac arrhythmias. To prevent this, your body will continuously pull from its vast intracellular and bone stores to “top off” the serum, masking a long-term depletion. This is why a serum magnesium test is a poor indicator of total body magnesium status—it shows the tightly regulated 1% in your blood, not the 99% in your cells and bones.
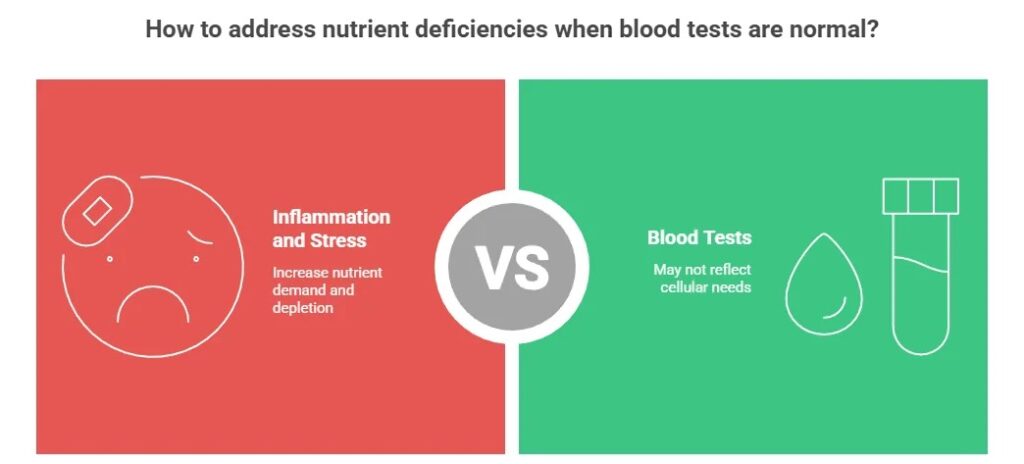
How does inflammation create a false normal reading?
During systemic inflammation, your liver produces acute phase proteins as part of the immune response. Key among these are ferritin (which binds iron) and ceruloplasmin (which binds copper). This process, called nutrient sequestration, intentionally lowers serum iron and zinc to “starve” invading pathogens. Unfortunately, it also makes these minerals less available to your own cells. So, in an inflamed state, you can have normal or even high serum ferritin (because it’s an acute phase reactant) while your cells are functionally deficient in iron, leading to fatigue and hair loss.
How do medications deplete cellular nutrients?
Many common drugs interfere with absorption or increase excretion, leading to gradual cellular depletion:
• Proton Pump Inhibitors (PPIs – e.g., omeprazole): Reduce stomach acid, critically impairing absorption of magnesium, Vitamin B12, and iron.
• Diuretics (“water pills”): Cause renal wasting of magnesium, potassium, zinc, and B vitamins.
• Metformin (for diabetes): Interferes with B12 absorption and cellular utilization.
• Oral Contraceptives: Can deplete B vitamins, magnesium, and zinc.
These depletions occur slowly over months or years and are rarely monitored with appropriate cellular-level testing.
Which nutrients are most likely to show a false normal?
The “Big Four” are Magnesium, Vitamin B12, Iron, and Vitamin D.
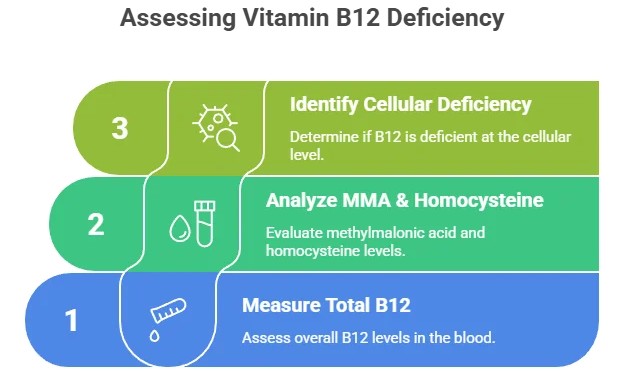
• Magnesium: The classic example. Serum tests miss ~99% of your body’s magnesium. Better test: RBC Magnesium. • Vitamin B12: Serum B12 can be misleading. Better markers: Methylmalonic Acid (MMA) and Homocysteine. • Iron: Serum iron fluctuates daily. Critical test: Ferritin (aim for >30 ng/mL for stores, >50 for optimal).
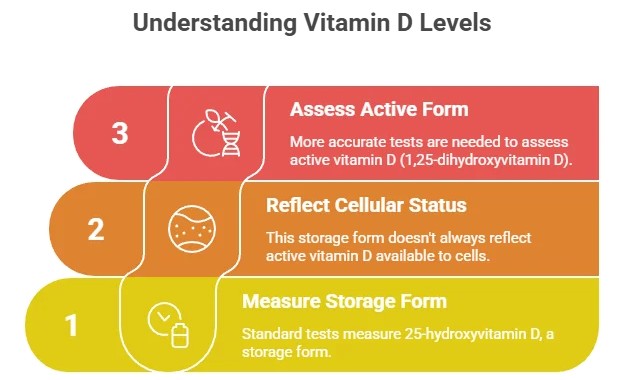
• Vitamin D: Standard 25-OH-D test doesn’t show the active hormone. Issues with receptor sensitivity also exist.
Others include Potassium, Zinc, and Active Folate (B9).
What are the real symptoms of low cellular magnesium?
Symptoms of cellular magnesium deficiency are widespread because magnesium is involved in over 300 enzymatic reactions:
• Muscular: Cramps, twitches, tension, poor recovery
• Neurological: Anxiety, insomnia, migraines, brain fog
• Cardiac: Palpitations, arrhythmias, high blood pressure
• Metabolic: Insulin resistance, fatigue, constipation
If you have these symptoms with a “normal” serum magnesium (especially if below 2.0 mg/dL), cellular deficiency is likely.
What specific tests can reveal a cellular deficiency?
Ask your practitioner about these more revealing tests:
1. Functional Cellular Tests: • RBC Nutrient Analysis: Measures magnesium, zinc, selenium, etc., inside red blood cells.
• SpectraCell or NutrEval: Assesses nutrient function within white blood cells over their lifespan.
2. Metabolic Marker Tests: • MMA & Homocysteine: Elevation indicates functional B12/folate deficiency at the cellular level.
• Organic Acids Test (OAT): Urine test showing metabolic byproducts; reveals blockages in cellular energy pathways.
3. Comprehensive Panels: • Full Thyroid Panel (TSH, Free T3, Free T4, Reverse T3, antibodies)
• Full Iron Panel (Serum Iron, TIBC, Ferritin, % Saturation)
How do I talk to my doctor about this?
Be prepared, collaborative, and symptom-focused:
1. Lead with symptoms: “I understand my labs are in range, but I’m still struggling with significant fatigue, muscle cramps, and brain fog.”
2. Ask informed questions: “Given my symptoms, could we explore if there’s a functional deficiency? I’ve read about RBC magnesium or MMA tests being more sensitive for cellular status. What are your thoughts?”
3. Suggest a trial: “Would you be open to a therapeutic trial of magnesium glycinate for 3 months to see if my symptoms improve, while we monitor?”
4. Get a referral: If needed: “Would a referral to an endocrinologist or functional medicine doctor who specializes in this area be appropriate?”
Bringing peer-reviewed articles can help, but focus the conversation on your persistent symptoms and seeking solutions.
What are “activated” or “bioavailable” supplements?
These are nutrient forms that are either already in the state your cells use or are more easily converted. They bypass potential genetic or metabolic bottlenecks:
• For B12: Choose Methylcobalamin or Adenosylcobalamin over cyanocobalamin.
• For Folate: Choose 5-MTHF (L-Methylfolate) over folic acid, especially if you have MTHFR variants.
• For Magnesium: Glycinate (calming, well-absorbed), Malate (energy), L-Threonate (brain).
• For Vitamin D: Always pair D3 with Vitamin K2 (MK-7) for proper calcium direction.
Quality matters. Look for reputable brands that use these superior forms.
Can I fix this through diet alone?
It depends on the depth of the deficiency and your individual absorption. Diet is the essential foundation. Prioritize magnesium-rich foods (pumpkin seeds, spinach, almonds), heme iron (red meat, organ meats), and B vitamins (pastured eggs, salmon).
However, if you have:
• Long-standing symptoms
• Genetic factors (like MTHFR)
• Gut health issues
• Medication-induced depletion
• High stress or inflammation
…diet alone may be insufficient to replete deep cellular stores. Strategic supplementation with bioactive forms, under guidance, is often necessary to correct the deficiency, after which an optimal diet can maintain levels.
Is this a way to sell expensive tests and supplements?
This is a critical and valid question. While the “False Deficiency” trap is a real, science-backed phenomenon, it can be exploited. Red flags: A practitioner who orders excessive expensive tests without clear rationale, pushes proprietary supplements exclusively, or dismisses all standard labs as worthless.
Green flags for a credible practitioner: • They start with a thorough history and review of your standard labs.
• They use advanced testing strategically to answer specific clinical questions.
• They explain the “why” behind each test and supplement.
• They focus on food-first approaches and root causes (gut health, stress).
• They welcome collaboration with your primary care doctor.
Your best defense is education. Understand why a test is being recommended and how the results will change the treatment plan.
Could this be a root cause of chronic illness?
Emerging research suggests it’s a significant contributing factor in many unexplained chronic conditions. Cellular nutrient deficiencies impair fundamental processes:
• Mitochondrial Function: Magnesium and B vitamins are co-factors for ATP (energy) production. Deficiency = fatigue.
• Detoxification Pathways: Glutathione production requires selenium, magnesium, and B vitamins.
• Methylation: Critical for DNA repair, neurotransmitter balance, and inflammation control; requires B12 and folate.
• Immune Regulation: Zinc and Vitamin D are crucial for immune cell function.
While not the sole cause, correcting cellular deficiencies is often a necessary step in resolving the metabolic dysfunctions at the heart of conditions like fibromyalgia, chronic fatigue syndrome, and certain mood disorders.
This phenomenon occurs when standard serum blood tests—the ones measuring nutrient levels in the liquid part of your blood—show “normal” ranges, while your cells are actually starving for essential vitamins and minerals. It’s a disconnect between what’s circulating in your bloodstream and what’s actually being utilized by your mitochondria, neurons, and muscles to produce energy and maintain health. Understanding this trap is crucial for anyone on a quest for genuine wellness, not just normal lab results.
Decoding the Jargon: Serum vs. Cellular Levels Explained Simply
To understand the false deficiency trap, let’s break down the key terms:
- Serum Levels: This is what a standard blood test measures. When a vial of blood is drawn and spun in a centrifuge, the red and white blood cells settle at the bottom. The clear, yellowish liquid on top is the serum. Serum tests measure the amount of a nutrient (like magnesium, Vitamin D, or B12) floating in this extracellular fluid, en route to your cells.
- Cellular Levels: This refers to the amount of a nutrient that has actually been transported inside your cells—into the mitochondria (your cellular power plants), the nucleus, and the cytoplasm—where the real biochemical work happens.

Think of it like this: The serum is the delivery highway, and your cells are the factories. A standard blood test counts how many nutrient “trucks” are on the highway. It can’t tell you if those trucks are actually getting into the factories, unloading their cargo, or if the factories are empty and shutting down. You can have plenty of trucks on the road (normal serum levels) but broken factory doors, leading to a cellular deficiency.
Why the Disconnect Happens: The 5 Root Causes of False Normals
Several complex biological factors can create this serum-cellular gap:
- The “Pooling” Problem & Homeostatic Control: The body prioritizes serum stability (homeostasis) for critical electrolytes. For potassium and magnesium, the body will rapidly leach these minerals from muscle and bone stores to maintain a normal serum level, even as severe intracellular deficits develop. This is why a patient can have a normal serum magnesium but suffer from ventricular arrhythmias due to myocardial magnesium deficiency.
- Transport & Absorption Breakdown (The Two-Gate Problem): Getting a nutrient from your gut into your blood (absorption) and from your blood into your cell (cellular uptake) are two distinct processes, each with potential failure points.
- Vitamin B12 requires intrinsic factor, a healthy ileum for absorption, and then the transcobalamin II transport protein for cellular delivery. Neurological damage from B12 deficiency can progress with serum levels in the low-normal range (often defined as 200-300 pg/mL) if cellular uptake is impaired.
- Insulin as a Co-Transport Hormone: Minerals like magnesium require adequate insulin sensitivity for cellular uptake. In insulin resistance (prediabetes, Metabolic Syndrome), cells may become resistant to magnesium entry, leading to intracellular deficiency despite normal serum levels—a factor that worsens the condition.
- The “Acute Phase Response” & Nutrient Sequestration: During systemic inflammation or infection, the liver produces acute phase proteins like ferritin and ceruloplasmin. These proteins actively sequester iron and zinc from the bloodstream, lowering serum zinc and iron (as part of the body’s defense to “starve” pathogens), while simultaneously making these minerals less available to your own cells. This creates a functional deficiency.
- Genetic Polymorphisms (SNPs) & Enzyme Function: Common genetic variations can dramatically affect nutrient metabolism at the cellular level.
- MTHFR gene variants can impair the conversion of dietary folate and synthetic folic acid into the active cellular form, 5-methyltetrahydrofolate (5-MTHF), disrupting methylation cycles critical for detoxification, neurotransmitter production, and DNA repair—all while serum folate levels appear normal.
- Variations in the VDR (Vitamin D Receptor) gene can affect how efficiently cells utilize Vitamin D, contributing to “high normal” serum levels with persistent deficiency symptoms.
- Drug-Nutrient Depletion & Interactions: Many common medications chronically deplete intracellular nutrient stores. Proton Pump Inhibitors (PPIs like omeprazole) reduce stomach acid, critically impairing absorption of magnesium, B12, and iron. Diuretics (like furosemide and HCTZ) cause renal wasting of magnesium, potassium, and zinc. Metformin can interfere with B12 absorption and cellular utilization. These depletions often occur gradually and are rarely monitored.
The Key Nutrients Most Often Misread by Serum Tests
Certain nutrients are notorious for this false normal phenomenon:
- Magnesium: The classic example. Symptoms of cellular magnesium deficiency include muscle cramps, anxiety, insomnia, migraines, and cardiac arrhythmias. A RBC Magnesium test is a more clinically relevant marker. Note that the serum magnesium reference range (1.7-2.2 mg/dL) may be too broad, with many patients symptomatic below 2.0 mg/dL.
- Vitamin B12 & Active Folate: Serum B12 has poor diagnostic sensitivity. Functional markers Methylmalonic Acid (MMA) and Homocysteine are metabolic proxies—if they are elevated, it indicates a functional B12 or folate deficiency at the cellular level, regardless of serum values. For folate, measuring RBC Folate assesses the body’s storage and cellular integration better than serum folate.
- Vitamin D: Beyond the standard 25-OH-D test, the active hormone 1,25-diOH-D can be insightful in autoimmune or inflammatory conditions. A high 1,25-D with a low-normal 25-D can indicate dysregulated conversion, often seen in granulomatous diseases.Absolute(intelli) Nutrition Rules
- Iron: The serum ferritin test is key. In non-inflammatory states, a ferritin level below 30 ng/mL is highly indicative of empty iron stores, even if hemoglobin and serum iron are normal. Clinically, patients (especially women) with ferritin between 15-50 ng/mL often present with significant fatigue, hair loss, and restless legs.
- Potassium & Zinc: Like magnesium, these are primarily intracellular. Hypokalemia (low serum K+) is a medical emergency, but patients with chronic, mild intracellular potassium deficiency can have normal serum levels and experience fatigue, weakness, and blood pressure dysregulation. For zinc, plasma or RBC zinc is a better marker than serum, though challenging to standardize.
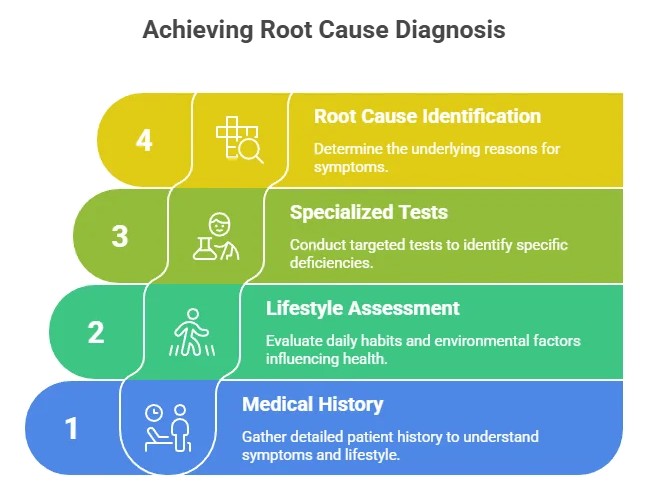
Beyond the Standard Panel: How to Test for True Cellular Health
If you suspect a false deficiency, what actionable steps can you take? The conversation with your healthcare provider is key. Here are more advanced testing options to discuss:
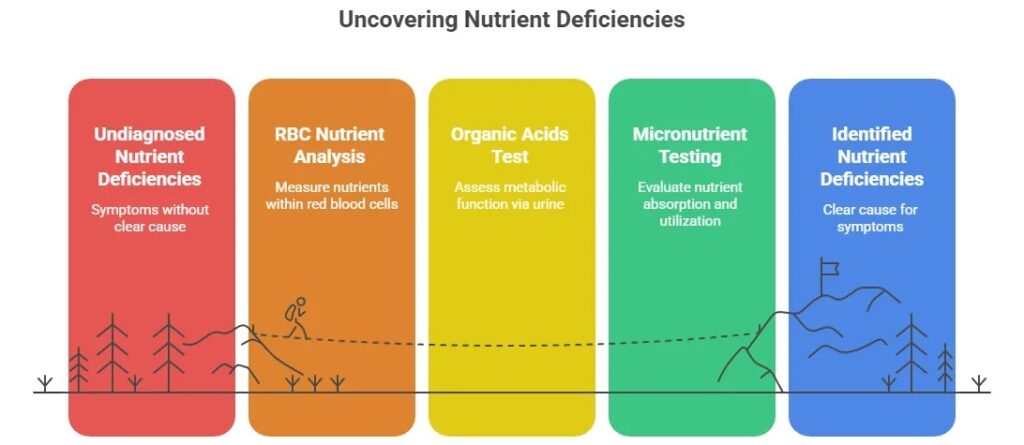
- Functional Nutrient Testing: These specialized tests assess cellular function and nutrient status.
- Comprehensive Nutrient Panels: Tests like SpectraCell’s Micronutrient Test or NutrEval by Genova Diagnostics measure functional deficiencies inside white blood cells, assessing how nutrients actually perform in supporting immune function and metabolic pathways.
- Organic Acids Test (OAT): This urine test analyzes metabolic byproducts. Elevated methylmalonate indicates B12 issues; high xanthurenate suggests B6 deficiency; and specific Krebs cycle markers can point to functional deficits in B vitamins, magnesium, and CoQ10.
- RBC Element Analysis: For minerals like magnesium, zinc, copper, and selenium, this provides a snapshot of what is incorporated into red blood cells over their 120-day lifespan, offering a medium-term status report.
- Comprehensive Thyroid Panel: A standard TSH test is insufficient. Free T3 (the active hormone) can be low while TSH is “normal,” indicating poor peripheral conversion (often due to stress, inflammation, or selenium deficiency). Reverse T3 can be elevated, indicating the body is blocking active thyroid hormone at the cellular level.
Bridging the Gap: Clinical and Lifestyle Strategies to Nourish Your Cells
Optimizing true cellular nutrition requires a targeted, often layered approach:
- Clinically-Informed Supplementation: Work with a practitioner to choose bioactive forms that bypass absorption/activation barriers.
- Magnesium: Use Magnesium Glycinate for general repletion, Malate for muscle pain/fatigue, and L-Threonate for cognitive support.
- B Vitamins: For those with MTHFR or elevated homocysteine, use activated forms: Methylcobalamin (B12), 5-MTHF (folate), and Pyridoxal-5-Phosphate (B6).
- Vitamin D: Always pair D3 with Vitamin K2 (MK-7) to ensure proper calcium metabolism and arterial health.
- Address Underlying Pathologies: Treat the root cause. This may involve:
- Gut Healing: Addressing SIBO, leaky gut, or low stomach acid (hypochlorhydria) to improve absorption.
- Managing Inflammation: Using diet, stress reduction, and targeted supplements (like omega-3s, curcumin) to lower the acute phase response and free up sequestered nutrients.
- Reviewing Medications: With a doctor, assess if drug-induced nutrient depletions can be mitigated with dose adjustment, alternatives, or strategic, monitored repletion.
- The Role of Co-Factors: Nutrients work in synergy. You cannot correct a magnesium deficiency without adequate B6, which is necessary for cellular uptake. Vitamin D activation requires magnesium. Iron recycling and thyroid function require adequate Vitamin A and copper. A holistic repletion strategy is essential.
- Monitor Clinical Response, Not Just Labs: The ultimate test is improvement in patient symptoms. Reduction in fatigue, improved sleep, resolution of muscle cramps, and clearer cognition are the most important markers that cellular nutrition is being restored.
Conclusion: Become the Expert of Your Own Body
The era of blindly trusting a standard lab printout is ending. The “False Deficiency” trap reveals a fundamental truth in functional and preventative medicine: Optimal health happens at the cellular level, not just in the bloodstream.
Your symptoms are valid data. If you feel unwell despite “normal” tests, you are likely experiencing a functional or cellular deficiency that standard medicine is currently missing. Advocate for yourself. Ask your doctor the right questions, explore more comprehensive testing if necessary, and adopt a lifestyle that focuses on nourishing the deepest level of your being—your cells.
By understanding that serum levels do not equal cellular levels, you empower yourself to move beyond chasing generic lab ranges and start pursuing genuine, vibrant health from the inside out. Don’t just settle for normal on paper. Strive for optimal in your life.
FAQs for the topic “The False Deficiency Trap:
❓ 1. Why do I feel unwell even though my blood tests are normal?
Standard lab ranges are designed to detect advanced disease, not early or functional imbalances. You may already have cellular stress, micronutrient depletion, inflammation, or hormonal shifts that haven’t crossed the clinical “disease” threshold yet—so your results appear normal, even though your body is struggling.
❓ 2. What is the “False Deficiency Trap”?
The False Deficiency Trap happens when blood tests show “normal” values, but those levels are not optimal for your body’s function. This leads to missed early deficiencies, delayed treatment, and ongoing symptoms such as fatigue, brain fog, muscle pain, hair loss, and poor immunity.
❓ 3. Which deficiencies are commonly missed in routine blood tests?
Commonly overlooked imbalances include:
- Vitamin B12 and folate (functional deficiency)
- Ferritin (iron storage)
- Vitamin D (optimal vs. minimal)
- Magnesium (intracellular levels not tested)
- Thyroid hormones (T3, reverse T3, antibodies not checked)
- Chronic inflammation markers (hs-CRP, homocysteine)
❓ 4. What is the difference between “normal” and “optimal” lab ranges?
- Normal range: Based on averages from the general population, including unhealthy individuals.
- Optimal range: Levels associated with peak cellular function and disease prevention.
You can be “normal” yet still far from optimal.
❓ 5. What should I do if my symptoms persist but my labs are normal?
You should consider a functional or regenerative medicine evaluation that looks at:
- Optimal ranges
- Nutrient status
- Mitochondrial health
- Hormone balance
- Inflammatory markers
This approach focuses on root cause correction, not just disease detection.
Medical Disclaimer
The information provided in this article is for educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment.
While the concepts discussed (including “false deficiency” and functional imbalances) are based on emerging research and clinical observations, they do not replace standard medical evaluation or care. Always consult a qualified physician or licensed healthcare provider regarding any symptoms, medical condition, or treatment decisions.
Do not disregard, delay, or avoid seeking medical advice because of something you have read here. Individual health needs vary, and what works for one person may not be appropriate for another.
If you are experiencing severe, persistent, or worsening symptoms, seek immediate medical attention.
Dr. Mohammed Abdul Azeem Siddiqui, MBBS, M.Tech (Biomedical Engineering – VIT, Vellore)
Registered Medical Practitioner – Reg. No. 39739
Physician • Clinical Engineer • Preventive Diagnostics Specialist
Dr. Mohammed Abdul Azeem Siddiqui is a physician–engineer with over 30 years of dedicated clinical and biomedical engineering experience, committed to transforming modern healthcare from late-stage disease treatment to early detection, preventive intelligence, and affordable medical care.
He holds an MBBS degree in Medicine and an M.Tech in Biomedical Engineering from VIT University, Vellore, equipping him with rare dual expertise in clinical medicine, laboratory diagnostics, and medical device engineering. This allows him to translate complex laboratory data into precise, actionable preventive strategies.
Clinical Mission
Dr. Siddiqui’s professional mission centers on three core pillars:
Early Disease Detection
Identifying hidden biomarker abnormalities that signal chronic disease years before symptoms appear — reducing complications, hospitalizations, and long-term disability.
Preventive Healthcare
Guiding individuals and families toward longer, healthier lives through structured screenings, lifestyle intervention frameworks, and predictive diagnostic interpretation.
Affordable Evidence-Based Treatment
Delivering cost-effective, scientifically validated care accessible to people from all socioeconomic backgrounds.
Clinical & Technical Expertise
Across three decades of continuous practice, Dr. Siddiqui has worked extensively with:
Advanced laboratory analyzers and automation platforms
• Cardiac, metabolic, renal, hepatic, endocrine, and inflammatory biomarker systems
• Preventive screening and early organ damage detection frameworks
• Clinical escalation pathways and diagnostic decision-support models
• Medical device validation, calibration, compliance, and patient safety standards
He is recognized for identifying subclinical biomarker shifts that predict cardiovascular disease, diabetes, fatty liver, kidney disease, autoimmune inflammation, neurodegeneration, and accelerated biological aging long before conventional diagnosis.
Role at IntelliNewz
At IntelliNewz, Dr. Siddiqui serves as Founder, Chief Medical Editor, and Lead Clinical Validator. Every article published is:
Evidence-based
• Clinically verified
• Technology-grounded
• Free from commercial bias
• Designed for real-world patient and physician decision-making
Through his writing, Dr. Siddiqui shares practical health intelligence, early warning signs, and preventive strategies that readers can trust — grounded in decades of frontline medical practice.
Contact:
powerofprevention@outlook.com
📌 Disclaimer: The content on IntelliNewz is intended for educational purposes only and does not replace personalized medical consultation. For individual health concerns, please consult your physician.